RCC Side Effect Management Guide
Side Effect Management Assistant
This tool helps you identify common side effects of advanced RCC treatment and provides practical management strategies. Select a side effect to see specific caregiver tips and guidance on when to contact your healthcare team.
Side Effect Information
Select a side effect from the dropdown above to view management information.
Symptom Tracker
Track symptoms daily to help your healthcare team adjust treatment as needed.
When a loved one receives a diagnosis of advanced renal cell carcinoma (RCC), the whole family can feel like the ground has shifted. The medical jargon, treatment decisions, and daily symptom flare‑ups create a whirlwind that caregivers often have to navigate alone. This guide breaks down what you need to know - from understanding the disease to handling side‑effects, emotional strain, and long‑term planning - so you can provide steady, compassionate support without losing yourself in the process.
What is Advanced Renal Cell Carcinoma?
Advanced renal cell carcinoma is a stage of kidney cancer where the tumor has spread beyond the kidney to distant organs such as the lungs, bones, or liver. According to the International Agency for Research on Cancer, RCC accounts for roughly 2% of all adult cancers and about 30% of newly diagnosed cases are already advanced at presentation. The disease is typically driven by mutations in the VHL gene, leading to uncontrolled blood vessel growth (angiogenesis) that fuels tumor expansion.
Key Symptoms and How They Evolve
The most common signs in advanced stages include persistent fatigue, unexplained weight loss, hematuria (blood in urine), and bone pain when the disease spreads to the skeleton. Breathlessness can arise from lung involvement, while abdominal swelling might signal ascites. These symptoms often fluctuate with treatment cycles, making consistent monitoring essential. Keeping a symptom journal - noting intensity, triggers, and timing - gives doctors concrete data to adjust therapy and helps caregivers anticipate needs.
Treatment Landscape in 2025
Modern care for advanced RCC centers on immunotherapy and targeted therapy. Checkpoint inhibitors like nivolumab and pembrolizumab unleash the immune system, while kinase inhibitors such as axitinib or cabozantinib block the pathways RCC uses to grow blood vessels. Combination regimens (e.g., pembrolizumab + axitinib) have shown median overall survival beyond 4 years in recent trials.
For patients meeting specific genetic criteria, newer agents like belzutifan - a HIF‑2α inhibitor - offer another line of attack. Clinical trials remain a vital option, especially when standard therapies plateau; trial enrollment can provide access to cutting‑edge drugs and close monitoring by specialist teams.
Managing Common Side‑Effects
Side‑effects often dictate quality of life more than the disease itself. Below is a quick‑reference table that outlines the most frequent adverse events and practical steps you can take.
| Side‑Effect | Typical Onset | Caregiver Tips |
|---|---|---|
| Fatigue | Weeks to months | Schedule low‑energy activities in the morning; encourage short, frequent rest periods. |
| Diarrhea | First 2‑4 weeks | Provide bland foods, oral rehydration salts, and note any medication changes. |
| Hypertension | Within 1 month | Monitor BP daily, reduce sodium, and coordinate with the oncology nurse for dose tweaks. |
| Skin rash | 2‑6 weeks | Use fragrance‑free moisturizers, cool compresses, and alert the team for possible steroid therapy. |
| Hand‑foot syndrome | 4‑8 weeks | Apply thick emollients, avoid tight shoes, and keep nails trimmed. |
Emotional Support: What Caregivers Need
Providing physical care is only part of the picture. Caregiver burnout is a real risk; studies from the American Cancer Society show that 40% of caregivers report moderate to severe stress after six months of continuous care. To safeguard your mental health:
- Set a regular check‑in time for yourself - even a 10‑minute walk can reset the nervous system.
- Share responsibilities with family members or hire a home‑health aide for respite.
- Join a kidney‑cancer support group (online forums like CancerCare or local hospital programs). Hearing others’ stories normalizes feelings and uncovers practical hacks.
Practical Day‑to‑Day Tips
Every day brings new tasks. Here are concrete actions that smooth the routine:
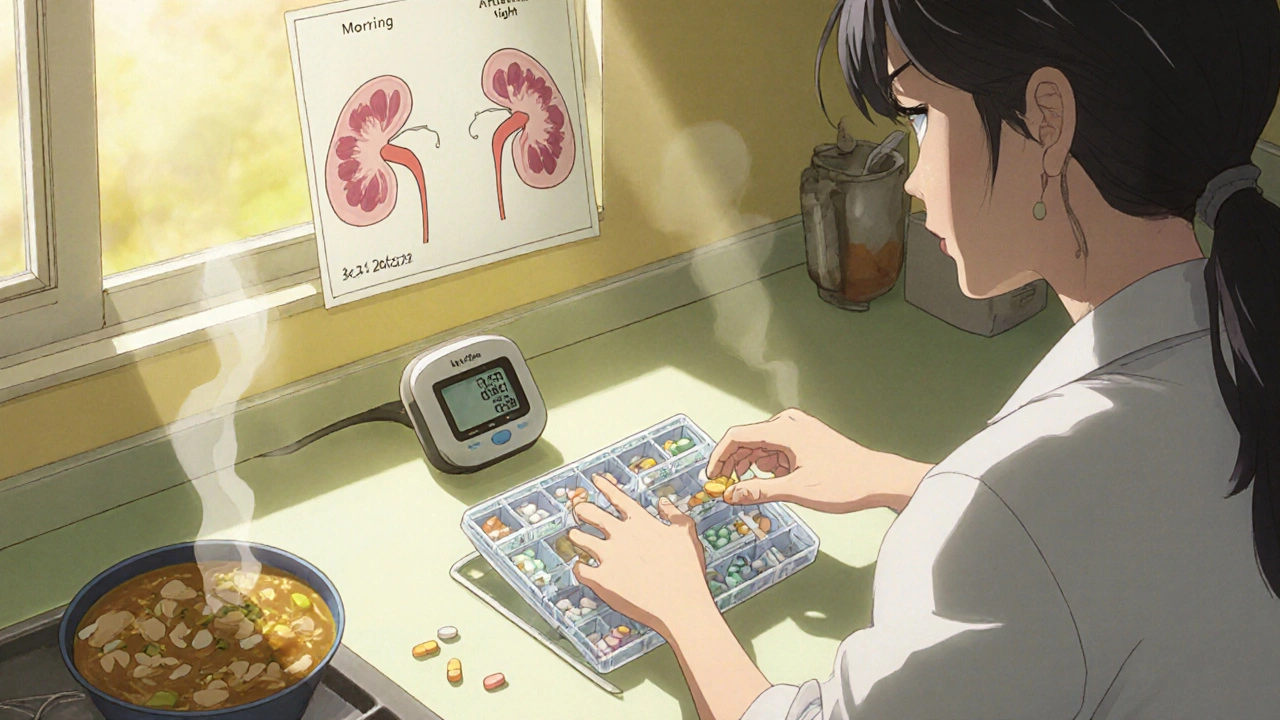
- Medication Management: Use a pill organizer categorized by morning, afternoon, and night. Keep a spreadsheet that records dose, time, and side‑effects observed.
- Appointment Coordination: Create a shared digital calendar (Google Calendar) with color‑coded entries for oncology appointments, labs, and imaging. Set reminders 48 hours in advance for fasting labs.
- Nutrition: Aim for high‑protein, low‑sodium meals. If taste changes occur, experiment with milder herbs, smoothies, or oral nutrition supplements like Boost + Protein.
- Hydration: Kidney patients often need careful fluid balance. Track intake in a simple app and discuss limits with the nephrology team.
- Home Safety: Remove tripping hazards, install handrails in the bathroom, and keep a bedside light on for night‑time bathroom trips.

Palliative and End‑of‑Life Planning
When the disease progresses despite therapy, palliative care becomes a cornerstone. Contrary to misconceptions, palliative care can start alongside active treatment, focusing on symptom relief, psychosocial support, and advance‑care directives. Discuss goals of care early - whether the priority is extending life, preserving function, or maximizing comfort.
Hospice services are available once curative options are exhausted. They provide 24‑hour nursing, pain management expertise, and bereavement counseling for families. Signing an advance directive and designating a health proxy ensures the patient’s wishes are honored, reducing decision‑making stress later on.
Resources for Caregivers
Finding reliable information early can prevent confusion. Trusted sources include:
- The Kidney Cancer Association (kidneycancer.org) - patient guides, webinars, and a caregiver toolkit.
- National Cancer Institute’s Cancer.Net - up‑to‑date treatment summaries and side‑effect checklists.
- ClinicalTrials.gov - searchable database for ongoing studies that accept patients with advanced RCC.
- Psychology Today’s therapist directory - search for oncology‑specialized counselors.
Don’t overlook financial assistance programs; many pharmaceutical companies offer co‑pay help for immunotherapy drugs, and nonprofit foundations can cover travel costs to specialty centers.
Frequently Asked Questions
How often should I expect lab tests for someone on targeted therapy?
Most oncologists order blood work every 2-4 weeks to monitor liver enzymes, kidney function, and blood pressure. Your doctor may adjust the interval based on stability.
What are the signs that a side‑effect needs urgent medical attention?
Severe shortness of breath, sudden high fever, uncontrolled bleeding, or a drastic rise in blood pressure (>180/110 mmHg) should trigger an immediate call to the oncology team or a visit to the emergency department.
Can my loved one continue working while on treatment?
It depends on fatigue levels and job demands. Many patients shift to part‑time or remote roles. Discuss flexibility options with the employer early on.
Is it safe to give over‑the‑counter pain relievers?
Acetaminophen is generally safe if liver function is normal, but NSAIDs (ibuprofen, naproxen) can worsen hypertension or kidney function. Always check with the oncology pharmacist.
How can I talk to my loved one about prognosis without causing panic?
Use honest, compassionate language. Focus on what can be controlled now (treatment plan, symptom relief) and invite the patient to share how they feel about future decisions. A joint meeting with the care team can help keep the conversation factual.
Walking the caregiver path for advanced renal cell carcinoma is demanding, but you don’t have to go it alone. By understanding the disease, staying organized, and leaning on professional and community resources, you can provide meaningful support while preserving your own wellbeing.
13 Comments
Harry Bhullar October 21 2025
Managing the daily rhythm of medication can feel like juggling a circus of pills.
Start by sorting doses into a weekly pill organizer with compartments labeled morning, noon, and night.
Pair each compartment with a sticky note that lists the expected side‑effects for that drug.
This visual cue cuts down on missed doses and lets you spot patterns when fatigue spikes.
Keep a simple spreadsheet on your phone; log the exact time you give the medicine and any reactions you notice.
When a new therapy is introduced, note the onset of hypertension or skin rash within the first two weeks.
If you see a trend, flag it for the oncology nurse before the next clinic visit.
Hydration is a silent hero-aim for at least eight ounces of fluid every four hours unless the nephrologist says otherwise.
Use a reusable water bottle with time markers to remind you to sip regularly.
Nutrition plays a big role too; high‑protein snacks like Greek yogurt or a handful of nuts can combat the catabolic state caused by the cancer.
If taste changes make food unappealing, experiment with mild herbs, pureed soups, or fortified shakes.
Exercise doesn’t have to be a marathon; a 10‑minute walk after lunch can improve circulation and mood.
Scheduling a brief “check‑in” with yourself each evening-just five minutes to breathe and jot down worries-helps prevent burnout.
Don’t hesitate to delegate tasks; ask a sibling to handle grocery runs or hire a home‑health aide for a few hours a week.
Lastly, remember that caring for yourself isn’t selfish; it’s the cornerstone that lets you stay present for your loved one.
Kimberly Lloyd October 21 2025
Every step you take toward structure becomes a quiet affirmation that you’re still in control, even when the disease feels chaotic.
Chirag Muthoo October 22 2025
It is advisable to maintain a logbook in a bound notebook, documenting medication times, observed adverse reactions, and any deviations from the prescribed regimen, thereby facilitating a clear communication channel with the treating oncologist.
Dana Yonce October 23 2025
Keep a daily hydration log, it really helps.
Lolita Gaela October 23 2025
From a pharmacologic perspective, integrating a checkpoint for blood pressure monitoring is essential when patients are on VEGF‑targeted TKIs such as axitinib; a systolic reading consistently above 140 mmHg warrants a dose adjustment or antihypertensive addition.
Simultaneously, the emergence of grade 2 hand‑foot skin reaction often signals adequate drug exposure, but may necessitate proactive emollient therapy and possible dose interruption.
Moreover, the utilization of oral rehydration solutions can mitigate treatment‑related diarrhoea, preserving electrolyte balance and preventing secondary renal compromise.
Embedding these protocols into a caregiver’s routine reduces emergency visits and improves overall treatment tolerability.
Giusto Madison October 24 2025
Listen up-if you’re not tracking side‑effects in real time, you’re basically flying blind while the oncologist is throwing darts at a moving target.
Grab a cheap notebook, jot down every headache, every blood pressure spike, every rash, and bring that damn list to the next appointment.
Don’t rely on memory; doctors love data, and the more you give them, the better they can tweak your loved one’s regimen.
And for God’s sake, schedule a weekly 10‑minute “reset” where you breathe, stretch, and check the calendar-otherwise you’ll burn out faster than a cheap candle.
Ivan Laney October 25 2025
It’s crystal clear that the American healthcare system should prioritize home‑based care to keep families together; outsourcing everything to distant specialists only fragments the support network.
We must demand that insurance plans fund in‑home nursing and tele‑oncology so that caregivers aren’t left stranded without resources.
Our nation’s strength lies in community resilience, and by reinforcing local care we uphold the very values that made this country great.
Sakib Shaikh October 25 2025
Yo, this whole kidney cancer thing is like a rollercoaster that never stops-one minute you’re on a new drug, the next you’re dealing with blood pressure spikes that feel like a thunderstorm in your veins!
And don’t get me started on the skin rash-seriously, it looks like I’ve been wrestling a bear!
But hey, we gotta keep pushing, ‘cause every day is a fight and we’re not giving up, no matter how dramattic it gets.
Angela Koulouris October 26 2025
Amid the whirlwind, remember to anchor yourself with short, purposeful breaks; a quick stretch or a sip of tea can rekindle your focus and keep the caregiving momentum alive.
erica fenty October 27 2025
Data‑driven approach-track labs, vitals, meds; cross‑reference; adjust; repeat; optimize; survive.
Xavier Lusky October 27 2025
Ever notice how the pharma giants roll out new “miracle” drugs just as patents on older meds expire? It’s no coincidence; the industry manipulates data to keep us dependent on ever‑rising costs.
Ashok Kumar October 28 2025
Oh, great, another checklist-because clearly the only thing missing from an already overwhelming schedule is a spreadsheet that reminds you to breathe.
Jasmina Redzepovic October 29 2025
Patriotic duty demands that we safeguard our families from the onslaught of invasive treatments by championing home‑based palliative care, which not only preserves cultural values but also curtails unnecessary medical expenditures imposed by the globalist health agenda.