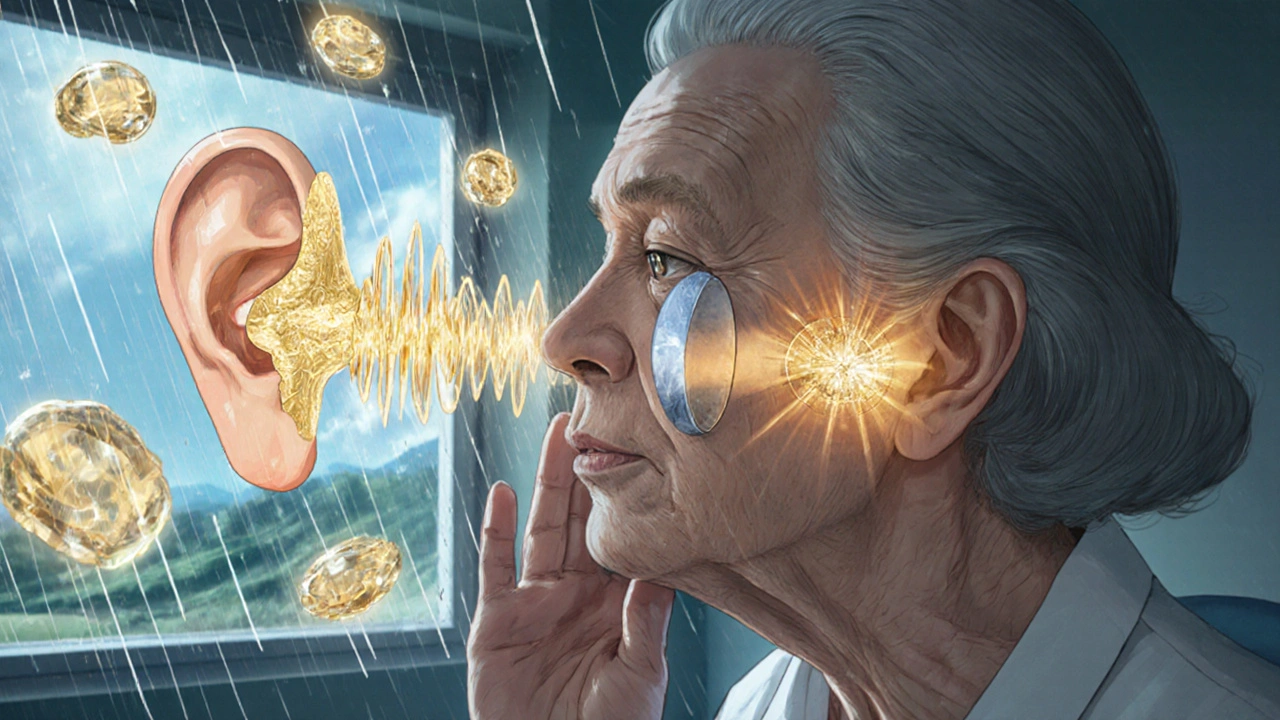
When you can hear people talking but everything sounds muffled-like they’re speaking through a wall-you might be dealing with conductive hearing loss. This isn’t just about being in a noisy room. It’s a physical blockage or damage in the outer or middle ear that stops sound from reaching the inner ear properly. Unlike sensorineural hearing loss, which affects the nerves or cochlea, conductive hearing loss is often fixable. And in many cases, surgery can restore hearing completely.
What Exactly Is Conductive Hearing Loss?
Conductive hearing loss happens when sound waves can’t move efficiently through the outer ear canal, eardrum, or the tiny bones in the middle ear (the ossicles: malleus, incus, and stapes). These structures are meant to amplify and transmit vibrations to the inner ear. When they’re blocked, stiff, or damaged, sound gets weaker. You might notice you need the TV louder than before, or you struggle to hear whispers or soft speech. Loud sounds don’t get clearer-they just get louder, but still fuzzy. This type of hearing loss can show up suddenly, like after a loud pop or ear injury, or it can creep in slowly over months. The key sign? An air-bone gap. That’s when your hearing is worse through air (like normal listening) than through bone (when sound is sent directly through the skull). Audiologists measure this gap using specialized tests. A gap of 15 to 60 decibels is typical. If it’s over 25-30 dB and lasts more than 3-4 months, surgery is often recommended.Common Middle Ear Problems That Cause It
Not all conductive hearing loss is the same. The cause determines the treatment. Here are the most common middle ear problems:- Otitis media with effusion (glue ear): Fluid builds up behind the eardrum without infection. It’s the #1 cause of hearing loss in kids. In the U.S., about 80% of children have at least one episode by age 3. The fluid dampens sound, making voices distant. Most cases clear up on their own, but if it lasts longer than 3 months, tubes may be needed.
- Perforated eardrum: A hole in the eardrum can come from trauma, infection, or loud noises. It affects 15-20% of adult cases. You might feel sudden pain, then hear better once the pain fades-but your hearing stays muffled.
- Otosclerosis: This is a genetic condition where the stapes bone (the smallest bone in the body) fuses to the inner ear wall. It doesn’t vibrate anymore. Hearing loss starts in your 20s or 30s, often getting worse over time. It’s more common in women and often runs in families.
- Cholesteatoma: This isn’t a tumor-it’s a skin cyst growing in the middle ear. It eats away at bone and can destroy the ossicles. It’s dangerous. Left untreated, it can lead to brain infections or permanent deafness. Surgery is always required.
- Aural atresia: A birth defect where the ear canal doesn’t form. It affects about 1 in 10,000 babies. Often, the middle ear structures are also underdeveloped. Hearing is severely limited from birth.
How Doctors Diagnose It
You can’t diagnose this yourself. Big-box hearing aid stores offer basic screenings-they can’t tell the difference between a clogged ear canal and a fused stapes bone. Proper diagnosis needs an audiologist and an ENT specialist. The process usually takes 2-4 weeks and involves:- Otoscopy: The doctor looks inside your ear with a lighted scope. Wax, fluid, or a hole in the eardrum is visible here.
- Audiometry: You wear headphones and press a button when you hear tones. This tests air conduction. Then, a small device behind your ear sends vibrations through bone. The difference between the two is the air-bone gap.
- Tympanometry: A probe changes pressure in your ear canal. If the eardrum doesn’t move, it suggests fluid behind it. Type B tympanograms (flat lines) mean fluid is present in 92% of cases.
- CT scan: For complex cases-like cholesteatoma or atresia-a high-resolution CT scan of the temporal bone shows bone structure in detail. Out-of-pocket cost in the U.S.? $800-$1,200.
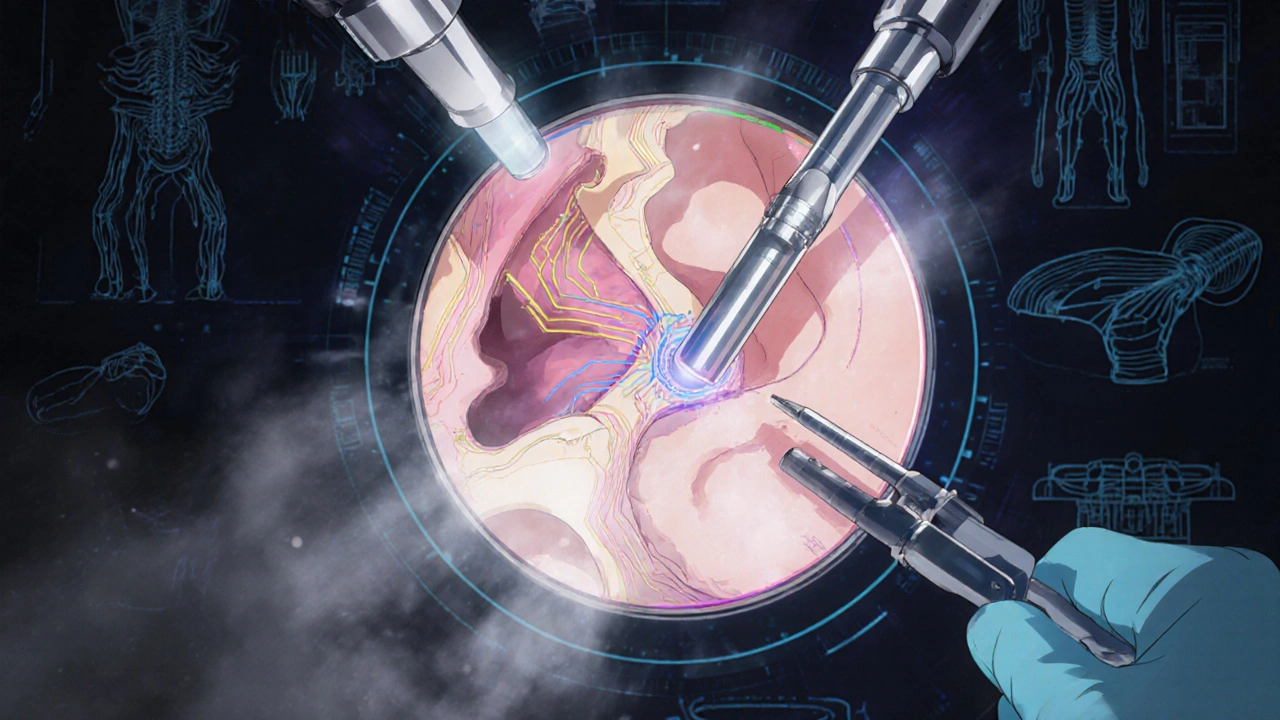
Surgical Repair Options
Surgery isn’t always the first step. For kids with glue ear, doctors often wait 3-4 months. For adults with mild wax buildup, cleaning alone fixes it. But when the problem is structural, surgery is the most reliable fix.Tympanoplasty for Perforated Eardrums
This surgery repairs a hole in the eardrum. The surgeon takes a graft-usually from your own tissue, like the temporalis fascia behind the ear-and patches the hole. Success rates? 85-95% for small perforations, 70-85% for larger ones. Recovery takes 6-8 weeks. You can’t get water in your ear. No flying. No heavy lifting. One patient told me: “I could hear birds again after 2 months. I didn’t realize how quiet my world had become.”Stapedectomy or Stapedotomy for Otosclerosis
This is one of the most successful ear surgeries ever done. The stapes bone is removed or modified with a tiny piston-like prosthesis. Modern laser-assisted techniques have cut complication rates from 15% to under 2%. Post-op, 80-90% of patients close their air-bone gap to within 10 dB. That means normal hearing. Side effects? Temporary dizziness (7%), altered taste (4%), or ringing in the ear (3%). One woman in her 40s said: “I heard my husband’s voice clearly for the first time in years. He cried.”Tympanostomy Tubes for Glue Ear
In kids, tubes are the go-to fix. A tiny hole is made in the eardrum, and a plastic tube is inserted. It lets fluid drain and air flow in. About 667,000 U.S. kids get them each year. Most infections stop within weeks. 75% of cases resolve in 3 months. Parents report 92% satisfaction. But 18% deal with persistent drainage, needing more antibiotics.Canalplasty for Aural Atresia
For babies born without an ear canal, surgeons rebuild the canal and sometimes the middle ear bones. It’s complex. Often, multiple surgeries are needed. Functional hearing improves in 60-70% of cases. But results vary. Some kids do better with bone-conduction hearing aids instead.Cholesteatoma Removal
This isn’t elective. It’s urgent. The cyst destroys bone. Surgery removes it and reconstructs the middle ear if possible. The goal? A safe, dry ear first. Hearing improvement is a bonus. Recovery takes 4-6 weeks. Many patients report “longer healing than expected.” 27% notice changes in sound quality afterward-everything sounds different, like the world has been re-tuned.What to Expect After Surgery
Recovery isn’t instant. You’ll need:- 6-8 weeks without water in the ear (no swimming, showers with ear protection)
- No flying or scuba diving for at least 8 weeks (pressure changes can ruin repairs)
- Avoid heavy lifting or straining
- Follow-up visits at 1, 3, and 6 months
Who Should Consider Surgery?
Surgery isn’t for everyone. But if you have:- A persistent air-bone gap over 25-30 dB
- Fluid or infection lasting 3-4 months
- A perforated eardrum that won’t heal
- Progressive hearing loss linked to otosclerosis
- Cholesteatoma (always)
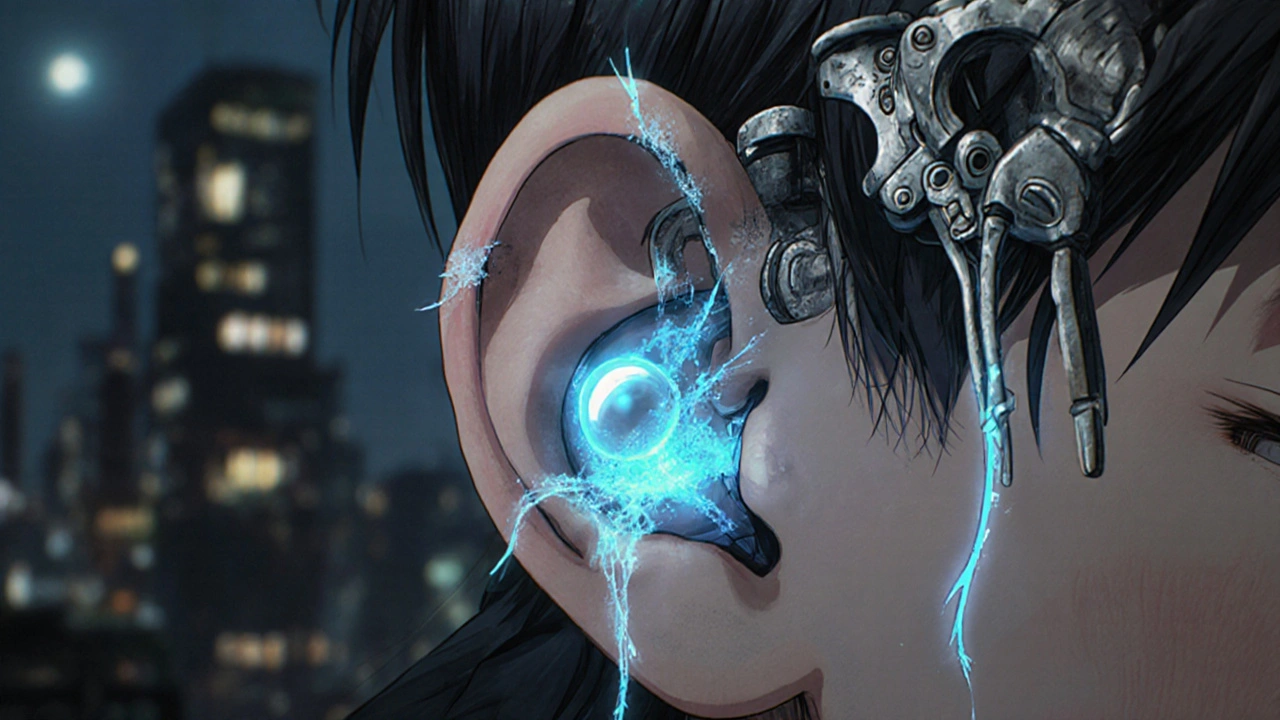
What’s New in Middle Ear Surgery?
Technology is improving outcomes fast:- 3D-printed ossicles: Custom-made tiny bones, printed from patient scans, fit perfectly. Early trials show 94% hearing improvement vs. 85% with standard implants.
- Endoscopic surgery: Instead of a large incision behind the ear, surgeons use a thin camera through the ear canal. Less trauma, faster recovery. By 2028, 60% of procedures are expected to use this method.
- Bioengineered grafts: New materials made from human tissue scaffolds are replacing old grafts. They integrate better-92% success rate vs. 85%.
- Intraoperative navigation: Like GPS for the ear. Used in 78% of U.S. ENT practices now. Reduces surgical errors by 35%.
Real Results, Real Risks
Patients who get surgery often report life-changing results. On patient forums, common comments: “I hear my granddaughter’s voice,” “I stopped missing phone calls,” “I finally enjoy music again.” But risks exist. Dizziness, taste changes, tinnitus, or incomplete hearing restoration can happen. Cholesteatoma patients sometimes need a second surgery if the cyst returns. Tympanoplasty grafts fail in 10-15% of cases. That’s why accurate diagnosis matters. You can’t fix what you don’t understand.When to See a Specialist
If you’ve had muffled hearing for more than a month, especially with:- Ear pain or drainage
- A history of ear infections
- Family history of hearing loss
- One-sided hearing loss
Can conductive hearing loss be cured without surgery?
Yes, in some cases. Earwax buildup, mild infections, or fluid in the middle ear often resolve with medication, ear drops, or time. In children, about 65% of conductive hearing loss cases improve without surgery. But if the cause is structural-like a fused bone, a hole in the eardrum, or a cholesteatoma-surgery is the only way to fix it.
How long does recovery take after middle ear surgery?
Recovery varies by procedure. For tympanoplasty or stapedotomy, most people return to light activities in 1-2 weeks, but full healing takes 6-8 weeks. You must avoid water, pressure changes, and heavy lifting during this time. Cholesteatoma surgery often requires longer recovery-4 to 6 weeks-because the procedure is more complex.
Is stapedectomy safe? What are the side effects?
Stapedectomy is one of the safest and most successful ear surgeries today. With modern laser techniques, complication rates are under 2%. Common side effects include temporary dizziness (7%), altered taste (4%), and worsening tinnitus (3%). Permanent hearing loss is rare-under 1%. Most patients report dramatic improvement in hearing within weeks.
Can children have middle ear surgery?
Yes. Tympanostomy tubes are the most common pediatric surgery in the U.S., with over 667,000 performed yearly. For children with chronic fluid or severe atresia, tympanoplasty or canalplasty may be done as early as age 2-3. Surgery is only recommended if hearing loss affects speech development or if infections don’t respond to treatment.
Will I need hearing aids after surgery?
Most people don’t. Surgery aims to restore natural hearing. But if the ear can’t be fully repaired-like in advanced cholesteatoma or severe atresia-bone-conduction hearing aids or implantable devices may be recommended afterward. These are not a backup-they’re a solution when anatomy won’t allow full recovery.
How do I know if my hearing loss is conductive or sensorineural?
Only an audiologist can tell for sure. Conductive hearing loss makes soft sounds hard to hear but doesn’t distort speech. Sensorineural loss makes speech sound muffled or unclear, even when loud. The key test is the air-bone gap: if air conduction is worse than bone conduction, it’s conductive. If both are equally poor, it’s sensorineural.
Are there non-surgical alternatives to improve conductive hearing loss?
Yes, but only for temporary or mild cases. Hearing aids can amplify sound, but they don’t fix the underlying problem. Bone-conduction devices (like BAHA or Osia) bypass the middle ear and send sound through the skull. They’re useful when surgery isn’t possible or failed. But for structural issues, surgery remains the most effective long-term solution.
15 Comments
Jauregui Goudy November 27 2025
Man, I never realized how much I was missing until I had my stapedotomy. I used to think my wife was mumbling, but turns out she was just talking normally. After surgery, I heard birds outside my window for the first time in 12 years. I cried in the parking lot. This isn’t just about hearing-it’s about coming back to life.
Don’t wait till it’s too late. If you’ve got that muffled feeling for more than a month, get it checked. No excuses.
Frances Melendez November 28 2025
Of course you’re all celebrating surgery like it’s some miracle cure. But have you considered that Big Pharma and ENT clinics are pushing this because it’s profitable? I’ve seen people get operated on and end up with worse hearing, dizziness for months, even taste loss. Why not just use hearing aids? Safer. Cheaper. Less invasive.
You’re all just drinking the Kool-Aid.
Lauren Zableckis November 29 2025
I appreciate how thorough this post is. I had glue ear as a kid and got tubes at age 5. My mom said I started saying ‘mama’ clearly for the first time the day after. I didn’t know then how much I’d been missing. Now I’m 34 and my hearing’s perfect-no surgery needed beyond those tubes.
It’s good to know what’s possible. Not everyone needs to go under the knife. But if you do, the science behind it is actually incredible.
Asha Jijen November 29 2025
so i had this thing where everything sounded like i was underwater and i thought it was just aging or my headphones being bad
turns out i had fluid for 6 months and my doc said if i waited another month i mighta needed surgery
just got ear drops and now i hear my dog barking like its right next to me
why do people jump to surgery so fast
also why is everything so long on here like its a textbook
Kaleigh Scroger November 30 2025
Let me tell you something about otosclerosis because I’ve lived it. My mom had it, my sister has it, and now I’m in my late 30s and starting to notice the same thing-voices sounding distant, music losing its texture.
I didn’t want surgery. I tried hearing aids. They made everything louder but still fuzzy. Like turning up a blurry TV.
Then I got the stapedotomy. The first thing I heard clearly? My own voice when I said ‘hello’ to the nurse. That’s when I knew. This wasn’t just improvement. It was restoration.
Yes there are risks. Yes you might get dizzy. But if you’re losing your ability to connect with people, you do what you have to do.
And if someone tells you ‘just wait and see’-they’ve never sat in silence while your kid says ‘I love you’ and you can’t quite catch it.
Don’t wait. Get tested. If the gap’s over 25 dB, you’re already behind.
Elizabeth Choi December 1 2025
Interesting how this post frames surgery as the default solution. But the data shows that 65% of conductive hearing loss in children resolves spontaneously. And for adults, many cases are just wax or transient fluid.
Why is the narrative so aggressively surgical? Is it because surgeons get paid per procedure? Why aren’t we talking more about conservative management as the first-line approach?
Also, 3D-printed ossicles? That’s not mainstream yet. This reads like a marketing brochure disguised as medical advice.
Iives Perl December 3 2025
They’re hiding the truth. The stapes prosthesis? It’s made with titanium from China. The CT scans? They use radiation to track you. And the ‘success rates’? All from studies funded by implant manufacturers.
Meanwhile, your ear canal is supposed to self-clean. If you’re getting fluid buildup, it’s because your body’s trying to detox from 5G towers.
Wear copper ear caps. Drink lemon water. Your body knows how to heal. Surgery is the trap.
Just saying.
Savakrit Singh December 3 2025
It is indeed an admirable exposition of the pathophysiological mechanisms underlying conductive hearing loss and the contemporary surgical interventions available. However, one must acknowledge the considerable economic disparities that render such procedures inaccessible to vast segments of the global population.
In India, for instance, a high-resolution CT scan costs more than three months’ salary for a laborer. The notion of ‘early intervention’ rings hollow when healthcare is privatized and unaffordable.
One wonders if the optimism regarding 3D-printed ossicles is not a luxury of the Global North.
Perhaps the true innovation lies not in prosthetics, but in equitable access.
Jebari Lewis December 5 2025
I’m a retired audiologist and I’ve seen everything. I used to work at a VA hospital. I had a veteran come in who hadn’t heard his daughter’s voice in 18 years because he had otosclerosis and thought hearing aids were ‘for old people.’
He got the stapedotomy. First thing he said after the bandage came off? ‘I can hear her laugh.’
Look-I’m not saying everyone needs surgery. But if you’ve got a persistent air-bone gap, you’re not just ‘a little hard of hearing.’ You’re missing out on human connection.
And yes, I typed that wrong. ‘Audiologist’ has two d’s. I know. I’m old. But I’m not wrong.
sharicka holloway December 6 2025
My cousin got tubes as a kid and now she’s a music teacher. She says she didn’t realize how much she missed until she heard a child sing in tune for the first time.
Don’t wait until you’re losing relationships because you keep saying ‘what?’
Go get your hearing tested. It’s free at a lot of clinics. No big deal. Just do it.
And if you’re scared of surgery? Talk to someone who’s been through it. Not a salesperson. A real person.
Alex Hess December 7 2025
Wow. So much effort spent glorifying a procedure that’s been around since the 1950s. The ‘success rates’ are inflated. The ‘life-changing’ testimonials? Cherry-picked. And 3D-printed ossicles? Still experimental. This reads like a paid ad from a surgical device company.
Real experts don’t write like this. They’d say ‘consider conservative management first.’
This is performative medicine.
Leo Adi December 7 2025
In India, my uncle had cholesteatoma. No one knew what it was. He went to three doctors before someone said, ‘This is not infection. This is growth.’
He got surgery in Delhi. Took two years to save his ear. Now he hears again. But he had to sell his cow.
So yes, surgery works. But not everyone can afford to live in a world where hearing is a privilege.
Thank you for writing this. But please remember: not all ears are the same. And not all lives have the same access.
Melania Rubio Moreno December 8 2025
so i think u meant 'conductive' not 'conductive' like in the title? or is that a typo? also why is everything so long i just wanted to know if my ear is clogged or if i need surgery
also i think u forgot to mention ear candles
Gaurav Sharma December 9 2025
How can you possibly recommend surgery without addressing the ethical implications of performing invasive procedures on children under the age of three? The eardrum is still developing. The ossicles are fragile. This is not ‘routine.’ This is experimentation dressed as care.
And the claim that 92% of parents are satisfied? With what? The fact that their child now has a plastic tube rattling in their skull? That’s not healing. That’s corporate medicine.
Shubham Semwal December 9 2025
Bro this is just basic ENT 101. You don’t need a 2000-word essay to say ‘if your ear is clogged see a doctor.’
Also why are you acting like stapedotomy is some new miracle? My grandma had it in 1987. She heard the radio again. Big deal.
And 3D printed bones? That’s sci-fi. You think a poor guy in Bihar can get that? Wake up.
Stop selling dreams. Just tell people to clean their ears and stop using headphones at 100%.