When a pregnant person takes a medication, it doesn’t just stay in their body. It travels through the bloodstream, reaches the placenta, and can cross over to the developing fetus. For decades, many assumed the placenta acted like a shield-keeping harmful substances out while letting nutrients in. But that’s not true. The placenta is not a wall. It’s a smart, selective gatekeeper. And sometimes, it lets drugs through-sometimes more than we expect.
The Placenta Isn’t a Barrier. It’s a Bridge.
The placenta weighs about half a kilogram at full term and has a surface area roughly the size of a small table-15 square meters. That’s not just for show. It’s designed for constant exchange: oxygen in, carbon dioxide out, glucose and amino acids flowing to the baby. But it also lets medications pass. How? Mostly through passive diffusion. If a drug is small, fat-soluble, and not tightly bound to proteins in the blood, it slips through easily.Take ethanol-alcohol. At just 46 daltons, it crosses the placenta almost instantly. Within 30 minutes of drinking, fetal blood alcohol levels match the mother’s. Nicotine, at 162 daltons, does the same. These aren’t exceptions-they’re examples of how simple physics governs what gets through.
But not all drugs follow the same rules. Large molecules like insulin (over 5,800 daltons) barely make it across. Less than 0.1% of maternal insulin reaches the fetus. That’s why insulin injections are safe in gestational diabetes-the baby doesn’t get flooded with it. But for smaller drugs, even ones we think of as harmless, the story changes.
Transporters: The Placenta’s Bouncers
The placenta isn’t just a passive filter. It has active systems-like bouncers at a club-that kick certain drugs back out. These are called efflux transporters. The two biggest players are P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP). They sit in the placental membrane and pump drugs back toward the mother’s side before they can reach the baby.Here’s what that looks like in real numbers: HIV medications like lopinavir, saquinavir, and indinavir are all pushed back by P-gp. In studies using human placental tissue, when researchers blocked P-gp, fetal exposure to these drugs jumped by 1.7 to 2.3 times. That’s huge. Without those transporters, more of the drug would reach the baby. But because they’re working, fetal concentrations stay low-sometimes as low as 1% of the mother’s level.
But here’s the catch: not all drugs are affected the same way. Digoxin, used for heart conditions, doesn’t get pushed back by P-gp. Even when you give a patient drugs like verapamil that block P-gp elsewhere in the body, digoxin still crosses the placenta at the same rate. That’s because digoxin doesn’t rely on P-gp. It uses a different path. This kind of specificity matters. It means you can’t assume one drug’s behavior predicts another’s.
When the Placenta Is More Permeable
Many people assume the placenta works the same way all through pregnancy. It doesn’t. In the first trimester, the barrier is looser. Tight junctions between placental cells aren’t fully formed yet. Efflux transporters like P-gp and BCRP aren’t fully expressed. That means drugs cross more easily early on.That’s why timing matters. A medication that’s risky in the first 12 weeks might be safer later. For example, thalidomide-used in the 1950s to treat morning sickness-caused severe limb defects only when taken during a narrow window in early pregnancy. The placenta wasn’t ready to block it. Today, we know that window exists for many drugs. That’s why the FDA now requires early assessment of placental transfer during drug development.
By week 28, the placenta has matured. Transporters are working harder. The barrier is tighter. But even then, it’s not foolproof. Drugs like methadone and buprenorphine still cross efficiently. Fetal concentrations reach 65-75% of maternal levels. That’s why babies born to mothers on these drugs often go through neonatal abstinence syndrome-withdrawal after birth.
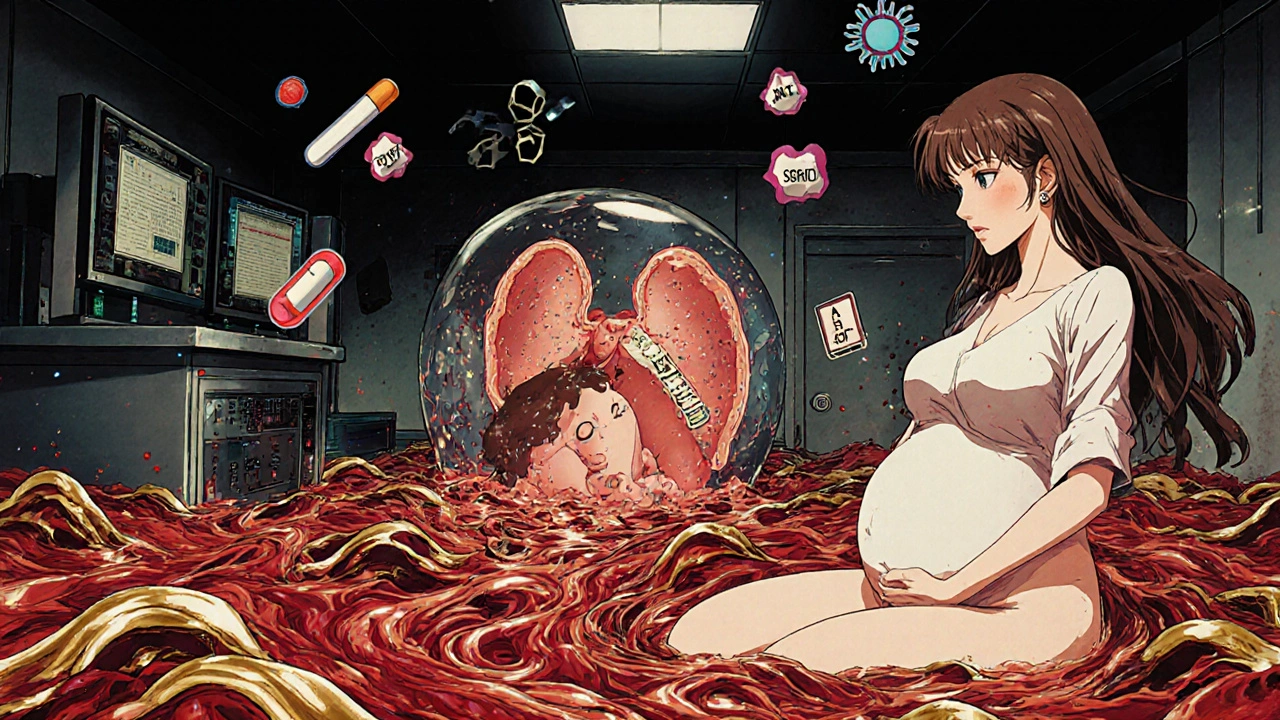
What Drugs Actually Reach the Fetus?
Some medications cross so well that fetal levels match or even exceed maternal levels. SSRIs like sertraline have cord-to-maternal ratios of 0.8 to 1.0. That means the baby gets nearly as much as the mother. About 30% of babies exposed to SSRIs in utero show temporary symptoms after birth: jitteriness, feeding problems, breathing issues. These usually resolve in days, but they’re real.Antiseizure drugs are another example. Valproic acid, used for epilepsy and bipolar disorder, crosses easily. Its cord-to-maternal ratio is 0.9-1.0. And it’s linked to a 10-11% risk of major birth defects-like spina bifida or heart problems-compared to just 2-3% in the general population. Phenobarbital does the same. It’s not the drug’s strength that matters. It’s how well it moves through the placenta.
Chemotherapy drugs are tricky. Paclitaxel, used for breast and ovarian cancer, crosses at 25-30% efficiency. But if you block P-gp, that number jumps to nearly 50%. That’s why doctors avoid certain chemo drugs in early pregnancy. Even if the mother needs treatment, the fetus might get too much.
What Blocks Drug Transfer?
Not everything gets through. Three things usually stop a drug from crossing: size, charge, and binding.Size: Anything over 500 daltons has a hard time. Most drugs under that threshold cross easily. That’s why insulin doesn’t-too big.
Charge: Drugs that are ionized (charged) at blood pH (7.4) don’t cross well. Why? The placental membrane is fatty. Charged molecules hate fat. So drugs like morphine (which can be charged) cross less than you’d expect based on size alone.
Protein binding: Only the free, unbound portion of a drug can cross. Warfarin is 99% bound to proteins in the blood. So even though it’s small and fat-soluble, almost none of it reaches the fetus. That’s why warfarin is still used in pregnancy for some conditions-though with extreme caution.
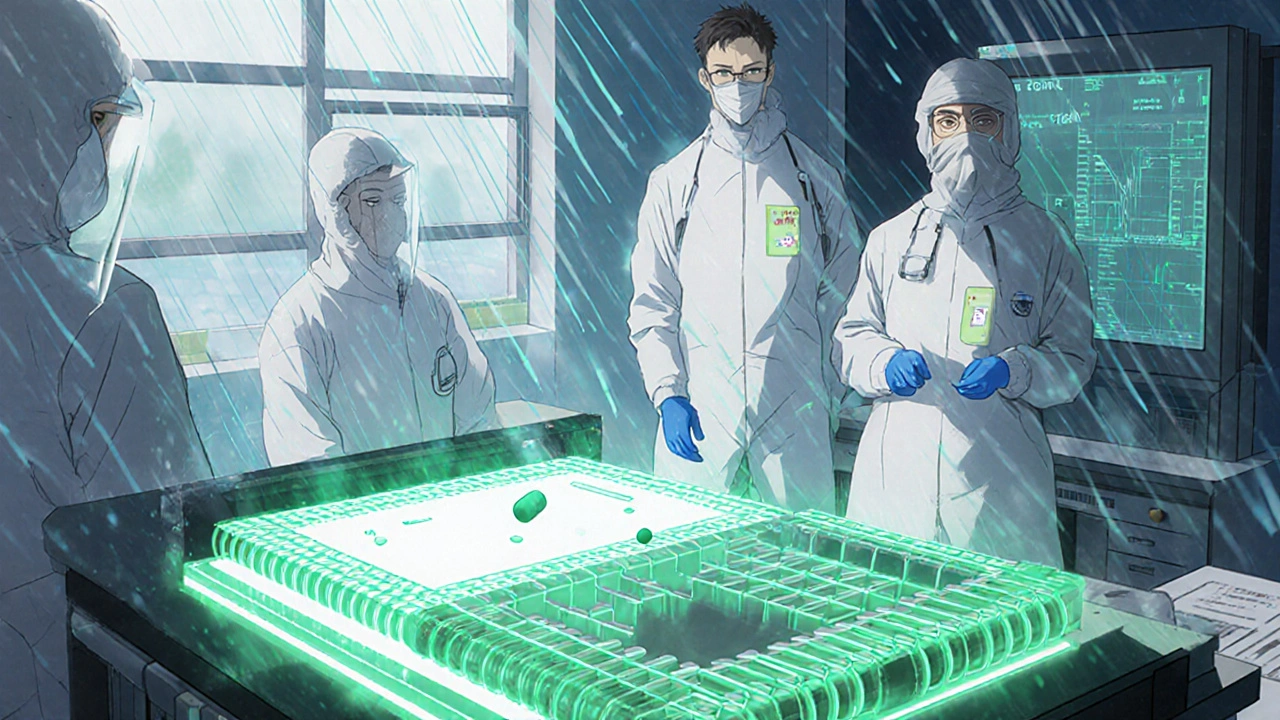
Why Animal Studies Don’t Tell the Whole Story
You might hear that a drug is safe because it was tested in mice. Don’t believe it. Mouse placentas are structurally different. They’re thinner. They have more blood vessels. And they let drugs through 3-4 times more easily than human placentas. A drug that looks harmless in a mouse study could be dangerous in a human pregnancy.That’s why researchers now use dually perfused human placentas-where they take a placenta after birth and pump fluids through both the mother and baby sides. It’s the gold standard. Even better are placenta-on-a-chip systems-microfluidic devices that mimic the placental barrier in a lab. One study showed glyburide (a diabetes drug) transfer rates of 5.6% in these chips-matching real placenta data within 1%. That’s accurate enough to guide clinical decisions.
What Does This Mean for Pregnant People?
If you’re pregnant and need medication, don’t stop cold turkey. But don’t assume everything’s safe either.Ask your doctor: “Does this drug cross the placenta?” and “Is there data on fetal outcomes?” For common drugs like acetaminophen, the answer is reassuring. For others-like certain antidepressants, antiseizure meds, or opioids-the answer is more complex.
Therapeutic drug monitoring helps. For drugs like digoxin or lithium, where the difference between a helpful dose and a toxic one is small, checking blood levels during pregnancy is critical. The placenta doesn’t change how much gets through, but your body does. You’re bigger. Your blood volume increases. Your kidneys clear drugs faster. Doses that worked before may not work now.
And if you’re on a drug with no clear safety data-about 45% of all prescription medications-you’re not alone. That’s why the FDA now requires placental transfer data for new drugs. But for older ones? We’re still catching up.
The Future: Targeted Therapy and New Risks
Scientists are now designing drugs that can cross the placenta on purpose-to treat fetal conditions like anemia or genetic disorders. Nanoparticles, tiny drug carriers, are being tested to deliver medicine directly to the fetus. But there’s a flip side. These particles might get stuck in the placenta, causing inflammation or long-term damage we don’t yet understand.There’s also growing interest in blocking transporters to help fetuses get more of a needed drug. Clinical trials for P-gp inhibitors to boost fetal exposure to antiviral drugs are starting in late 2024. It’s promising-but risky. We’re playing with a system we don’t fully control.
The thalidomide disaster taught us the placenta isn’t a shield. Today’s research shows it’s a dynamic organ that changes with time, responds to stress, and reacts to drugs in unpredictable ways. We’re learning more every year. But the bottom line hasn’t changed: every medication you take during pregnancy has the potential to reach your baby. That’s why informed choices matter.
Do all medications cross the placenta?
No. Whether a medication crosses depends on its size, fat solubility, charge, and how tightly it binds to proteins in the blood. Small, fat-soluble, uncharged drugs like alcohol, nicotine, and sertraline cross easily. Large or highly protein-bound drugs like insulin or warfarin cross very little. The placenta also has active transporters that push some drugs back out.
Is it safe to take antidepressants during pregnancy?
Some antidepressants, like sertraline, cross the placenta but are considered among the safest options. About 30% of babies exposed to SSRIs show temporary symptoms like irritability or feeding trouble after birth, but these usually resolve within days. Untreated depression carries its own risks, including preterm birth and low birth weight. Decisions should be made with your doctor based on your individual needs and the specific medication.
Why are some drugs riskier in the first trimester?
The placenta is still developing in the first trimester. Efflux transporters like P-gp and BCRP aren’t fully active yet, and the barrier between mother and baby is thinner. This makes it easier for drugs to reach the fetus during critical organ formation. That’s why drugs like thalidomide and valproic acid cause birth defects only if taken early-timing matters more than dose.
Can I take painkillers like ibuprofen while pregnant?
Acetaminophen (paracetamol) is generally considered the safest pain reliever during pregnancy. Ibuprofen and other NSAIDs are not recommended after 20 weeks because they can reduce amniotic fluid and affect fetal kidney development. Before 20 weeks, occasional use may be okay under medical supervision, but long-term or high-dose use increases risks. Always check with your provider.
How do I know if a drug is safe in pregnancy?
Look for updated labeling under the FDA Pregnancy and Lactation Labeling Rule (2015). It replaced the old A, B, C, D, X categories with detailed summaries on fetal risk, clinical considerations, and data sources. Talk to your doctor or pharmacist. Don’t rely on outdated sources or internet forums. If a drug has no clear data, it doesn’t mean it’s dangerous-it means we don’t know yet.

10 Comments
David Barry November 13 2025
The placenta isn't a wall it's a bouncer with a PhD in pharmacokinetics and honestly that's way more terrifying than any myth about it being a shield. Passive diffusion plus active efflux transporters? That's not biology that's a fucking security system designed by a rogue AI.
Alex Ramos November 13 2025
This is one of the clearest explanations I've ever read. Seriously. I work in OB/GYN and even I learned a few things. The P-gp stuff blew my mind. Thanks for breaking it down without dumbing it down. 🙏
edgar popa November 13 2025
so like... if i took tylenol last night is my baby gonna be fine?
Eve Miller November 14 2025
It’s not just about pharmacokinetics-it’s about moral responsibility. Every pill taken during pregnancy is a gamble with a human life. If you can’t prove it’s 100% safe, you shouldn’t take it. Period.
Benjamin Stöffler November 15 2025
Let’s be clear: the placenta is not a gatekeeper-it’s a compromised firewall. You’re not ‘filtering’ anything-you’re just delaying the inevitable. The fetus isn’t a separate entity-it’s an extension of maternal physiology, and any attempt to anthropomorphize the placenta as a ‘smart’ organ is just poetic nonsense wrapped in biobabble. Passive diffusion doesn’t care about your feelings. It obeys Fick’s law, not ethics. And yes, I’ve read the 2023 Nature review on placental transporter expression dynamics-so don’t patronize me with ‘it’s complicated’-it’s just physics with extra steps.
Mark Rutkowski November 16 2025
There’s something beautiful about how life finds a way-even through the most fragile, dynamic barriers. The placenta isn’t just a filter; it’s a conversation between two bodies, negotiating survival in real time. It’s not perfect-but it’s astonishing. And the fact that we’re finally building chips that mimic it? That’s not science fiction. That’s the future of compassionate medicine.
Ryan Everhart November 17 2025
So… you’re telling me the same thing that lets alcohol through also blocks insulin? And we’re surprised when drugs behave differently? I mean… we’ve known this since the 80s. Why does this feel like a revelation? Did we just forget everything we learned because it didn’t fit a nice narrative?
Chrisna Bronkhorst November 18 2025
Let’s cut the sentimentality. The placenta is a biological bottleneck with variable efficiency. It doesn’t care about your anxiety. It doesn’t care if you’re ‘informed.’ It’s a lipid bilayer with a few pumps. The real danger isn’t the drugs-it’s the delusion that we can predict outcomes. We’ve got 45% of meds with zero data. That’s not ‘we’re catching up’-that’s systemic negligence dressed up as science.
Amie Wilde November 20 2025
My OB said tylenol’s fine. I’m just gonna keep taking it. No stress. Baby’s gonna be fine. 😌
Alex Ramos November 21 2025
Just saw this reply and wanted to add-yes, acetaminophen is still the gold standard for pain relief in pregnancy. But even that’s not risk-free with long-term use. Recent studies link high-dose, prolonged exposure to possible neurodevelopmental effects. So yes, you’re probably fine-but ‘probably’ isn’t ‘guaranteed.’ Always dose low and talk to your provider. 💊