What is perioral dermatitis?
Perioral dermatitis is a red, bumpy rash that shows up around the mouth, often spreading to the area near the nose and eyes. It looks like small red bumps or tiny pus-filled spots, but unlike acne, there are no blackheads or whiteheads. Also known as periorificial dermatitis, it mostly affects women between 16 and 45, with men rarely getting it-about 9 out of 10 cases are female.
The rash usually spares the very edge of the lips, leaving a thin border of normal skin. Many people feel a burning or stinging sensation, and some report itching. In severe cases, the rash can spread to the skin around the eyes, making it even more noticeable and uncomfortable.
It’s not contagious. You can’t catch it from someone else. But it can last for months-or even years-if you don’t figure out what’s causing it. About 78% of people with this condition say it affects their confidence and makes them avoid social situations. That’s not just a skin issue-it’s a quality-of-life issue.
What triggers perioral dermatitis?
The biggest trigger by far is topical corticosteroids. That includes over-the-counter hydrocortisone creams, prescription steroid creams, and even some face creams that secretly contain steroids. About 85% of people with perioral dermatitis used these products before the rash appeared.
Here’s how it works: you put the cream on, the redness fades quickly, and you think it’s working. But when you stop, the rash comes back worse than before. This rebound effect happens in 92% of people who used steroids for more than two weeks. It’s a trap-what feels like relief is actually making things worse long-term.
Other common triggers include:
- Heavy moisturizers with petroleum jelly, dimethicone, or beeswax-these clog pores and trap irritation. About 45% of cases are linked to these ingredients.
- Fluoridated toothpaste-especially those with sodium fluoride at 1,000-1,500 ppm. Around 37% of people see improvement after switching to non-fluoride toothpaste.
- Makeup foundations-particularly those with comedogenic oils like isopropyl myristate. About 68% of cosmetic-related flare-ups come from foundation.
- Physical sunscreens with zinc oxide or titanium dioxide above 10% concentration. These can irritate sensitive skin in 22% of cases.
- Hormonal changes-many women notice the rash gets worse before their period. Oral contraceptives contribute in about 28% of female cases.
- Environmental factors-wind and sun exposure worsen symptoms in 41% and 63% of cases, respectively.
- Dental fillings and chewing gum-less common, but still reported in 12% and 19% of cases.
There’s also a link to Demodex mites-tiny bugs that live on everyone’s skin. They’re found in 83% of perioral dermatitis cases, compared to 45% in people without the rash. But whether they cause the problem or just hang out where the skin is already irritated is still debated.
What does gentle skin care look like?
Gentle skin care for perioral dermatitis isn’t about using more products-it’s about using the right ones, and using fewer of them.
Start by stopping everything. That means no creams, no serums, no exfoliants, no retinoids, and no acne treatments. Your skin needs to reset.
Cleansing
Wash your face only once a day-preferably at night. Twice-daily washing dries out the skin barrier and makes the rash worse in 88% of cases.
Use a non-foaming, pH-balanced cleanser with a pH between 5.5 and 6.5. Foaming cleansers contain sulfates that strip the skin. Look for ingredients like glycerin or ceramides. Cetaphil Gentle Skin Cleanser is one of the most commonly recommended.
Moisturizing
Moisturizer isn’t optional-it’s essential. But most moisturizers make this condition worse.
Choose a lightweight cream with:
- Ceramides between 0.5% and 2%
- Hyaluronic acid under 1%
- No petrolatum, dimethicone, or beeswax
Vanicream Moisturizing Cream is a top pick because it’s fragrance-free and has just enough ceramide to repair the barrier without clogging pores.
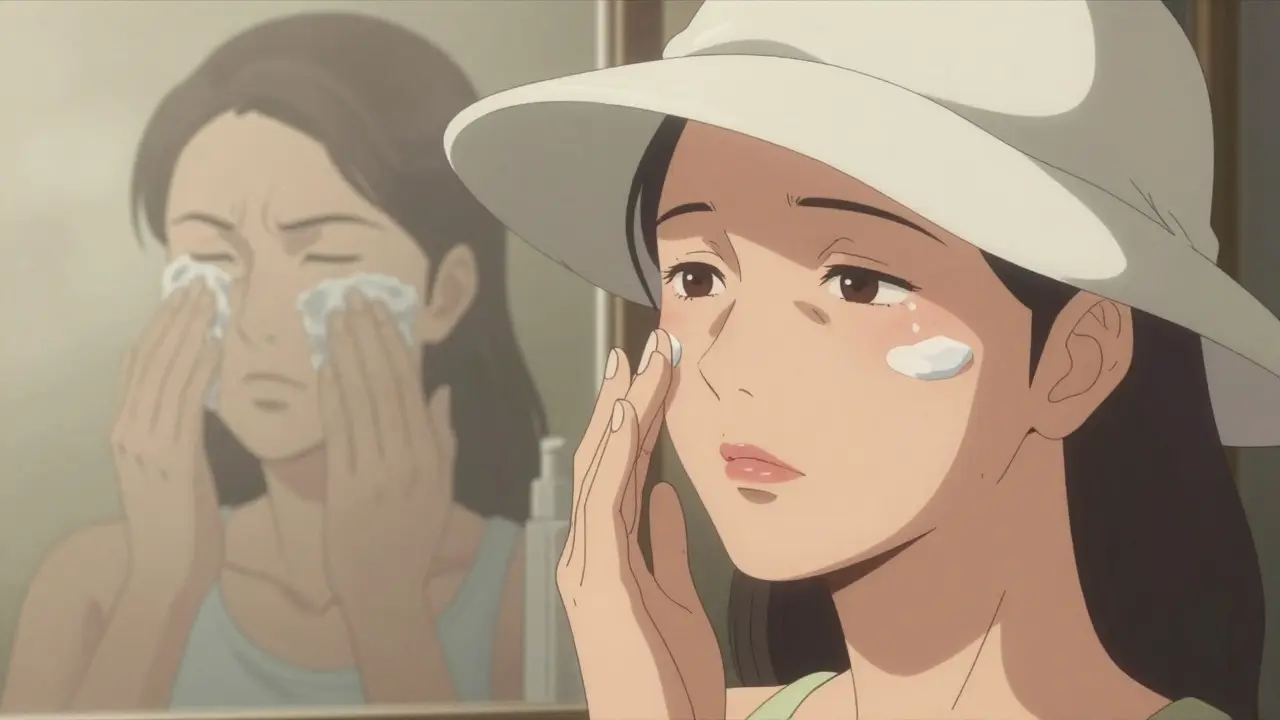
Sun protection
You still need sunscreen. But heavy mineral sunscreens with zinc oxide or titanium dioxide above 5% can trigger flare-ups in 31% of people.
Look for liquid or gel sunscreens with mineral filters below 5%. EltaMD UV Clear Broad-Spectrum SPF 46 (with 4.7% zinc oxide) is frequently mentioned by patients as a winner.
Alternatively, wear a wide-brimmed hat. Physical barriers are safer than any sunscreen for sensitive skin.
Makeup
If you must wear makeup, go for:
- Fragrance-free
- Non-comedogenic
- Titanium dioxide under 3%
- No isopropyl myristate
Mineral tinted moisturizers are often better than full-coverage foundations. Some people find they can skip makeup entirely during healing-and that’s perfectly fine.
Toothpaste
Switch to a non-fluoridated toothpaste with sodium lauryl sulfate (SLS) under 0.1%. Many people notice improvement within 4-6 weeks. Brands like Tom’s of Maine Fluoride-Free or Sensodyne Pronamel Gentle Whitening (SLS-free) are good options.
Medical treatments that actually work
While gentle skin care is the foundation, some cases need medical help.
Topical metronidazole 0.75% gel clears the rash in 70% of patients after 8 weeks. It’s applied twice daily and has minimal side effects.
Pimecrolimus 1% cream (an immunomodulator) works in 65% of cases and doesn’t carry the risk of antibiotic resistance. It’s often used when antibiotics don’t work or aren’t preferred.
For moderate to severe cases, oral doxycycline 40mg modified-release is now the standard. It’s much gentler than the old 100mg doses. Studies show 85% clearance after 12 weeks, with only 12% of patients reporting stomach upset-compared to 45% with higher doses.
Treatment usually takes 6-12 weeks. Stopping too early leads to a 40% chance of the rash coming back. Patience is key.
What doesn’t work-and why
Many people try home remedies: apple cider vinegar, tea tree oil, aloe vera, or coconut oil. These can make things worse. Coconut oil is occlusive. Tea tree oil is an irritant. Vinegar changes your skin’s pH and strips the barrier.
Even “natural” doesn’t mean safe. Perioral dermatitis is not caused by dirt. Scrubbing, exfoliating, or using acids (like glycolic or salicylic) will only damage your skin more.
Also, don’t be fooled by products labeled “for sensitive skin.” That term isn’t regulated. Always check the ingredient list.

Real patient stories
On Reddit’s r/SkincareAddiction, hundreds of people share their journeys. The most common pattern? A 3-4 week period of worsening symptoms after stopping steroids. They call it “the flare.” It’s scary. But 78% say it gets better after that.
One woman from Manchester wrote: “I used hydrocortisone for a month thinking it was eczema. When I stopped, my face looked like it had been set on fire. I cried every day for two weeks. Then, slowly, the bumps faded. Now I use only two products-and I haven’t had a flare in 11 months.”
Another said: “I switched toothpaste and noticed the rash around my mouth started shrinking within 10 days. I didn’t even need medication.”
These aren’t outliers. They’re the rule.
How to prevent it from coming back
Recurrence is common-up to 60% if triggers aren’t fully removed. But with proper education, that drops to 25%.
Here’s how to stay clear:
- Never use steroid creams on your face again-even if you think you need them.
- Stick to your gentle routine: one cleanser, one moisturizer, one sunscreen.
- Check every product label for hidden steroids, oils, or SLS.
- Replace your toothpaste and avoid chewing gum if it triggers you.
- Wear a hat in strong sun or wind.
- Be patient. Healing takes time.
Dietary changes like going gluten-free help in some cases-43% of patients with gluten sensitivity see improvement. But for most, it’s not the main issue. Don’t cut out entire food groups unless you have a confirmed sensitivity.
When to see a dermatologist
You don’t need to suffer alone. If the rash lasts more than 2 weeks, gets worse, or spreads to your eyes, see a dermatologist. They can confirm the diagnosis and rule out rosacea, acne, or fungal infections.
Bring your product list. Write down what you’ve used in the last 3 months. That’s often the missing piece.
Remember: this isn’t your fault. It’s not because you’re not cleaning well enough. It’s not because you’re using the wrong brand. It’s a reaction to specific triggers-and once you know them, you can fix it.
Can perioral dermatitis go away on its own?
It can, but only if you remove the triggers. Most people don’t realize they’re using steroids or irritating products, so the rash keeps coming back. Without change, it often lasts months or years. Stopping the triggers and using gentle care gives you the best chance for lasting relief.
Is perioral dermatitis the same as acne?
No. Acne has blackheads and whiteheads (comedones), while perioral dermatitis doesn’t. The bumps in perioral dermatitis are smaller, often red or pink, and form a ring around the mouth. It also doesn’t respond to acne treatments like benzoyl peroxide or retinoids-in fact, those make it worse.
How long does it take to heal?
Most people see improvement within 2-4 weeks after stopping steroids and switching to gentle products. Full healing usually takes 6-12 weeks. The first 7-14 days are often the worst, with increased redness and bumps-this is called the rebound flare. It’s normal, but it’s not the end. Stick with it.
Can I use makeup while I have perioral dermatitis?
It’s best to avoid it during the healing phase. If you must wear makeup, choose only fragrance-free, non-comedogenic products with titanium dioxide under 3%. Mineral tinted moisturizers are safer than heavy foundations. Many people find they don’t need makeup at all after a few weeks of healing.
Why does my skin get worse when I stop using steroid cream?
Steroid creams suppress inflammation temporarily, but they weaken your skin’s natural barrier over time. When you stop, your skin goes into overdrive trying to recover, which causes a rebound flare. This is called steroid-induced dermatitis. It’s not a sign you’re doing something wrong-it’s a sign your skin is healing. The flare usually peaks at 7-14 days and then improves.
Are there any natural remedies that work?
Most natural remedies-like coconut oil, tea tree oil, or apple cider vinegar-can irritate sensitive skin and make perioral dermatitis worse. There’s no strong evidence that any natural treatment cures it. The most effective approach is removing triggers and using simple, gentle products backed by clinical studies.
Can children get perioral dermatitis?
Yes, though it’s less common. In children, it’s often linked to steroid creams used for eczema or diaper rash. The treatment is the same: stop the steroids, use gentle cleansers, and avoid heavy moisturizers. Always consult a pediatric dermatologist for kids.

15 Comments
Meenakshi Jaiswal December 19 2025
I had this for over a year and thought it was acne. Switched to Cetaphil and Vanicream after reading this - no steroids, no fancy serums. Just clean water and patience. 8 months clear now. You got this.
Connie Zehner December 20 2025
OMG I KNEW IT!! I told my dermatologist like 3 times that fluoride toothpaste was the issue but she just kept giving me antibiotics 😭 I switched to Tom's fluoride-free and within 10 days my chin stopped looking like a battlefield 🙌
mark shortus December 21 2025
Okay so let me get this straight... you're telling me that the entire skincare industry is built on lies and that the only thing that works is... NOT using anything? I mean... wow. I feel like I've been scammed by 17 different brands and my entire identity as a 'skin guru' is now in shambles. 😭
Nina Stacey December 23 2025
I just want to say that I'm so proud of everyone who's been through this because it's not easy to stop using all those creams you think are helping you and just sit there and let your skin scream at you for two weeks but i did it and i cried a lot and i almost went back to the hydrocortisone but i didn't and now my skin is soft and calm and i feel like a new person like seriously like i can go outside without a hat and it's not because i'm brave it's because i finally trust my skin again
Dominic Suyo December 23 2025
Let’s be real - this is just steroid withdrawal dressed up as a skincare guide. The real issue? We’ve been conditioned to treat inflammation like a crime scene. The skin doesn’t need ‘repair’ - it needs space. And yes, zinc oxide at 10% is basically sandpaper for compromised barriers. But let’s not pretend this isn’t a systemic failure of dermatology’s lazy diagnostic habits.
Danielle Stewart December 25 2025
I’ve been following this protocol for 10 weeks now. No makeup. No moisturizer except Vanicream. No fluoride toothpaste. And guess what? My skin isn’t perfect - but it’s quiet. And that’s more than I’ve had in 5 years. Thank you for the clarity.
mary lizardo December 26 2025
The author’s assertion that 'natural' remedies are universally harmful is both reductive and scientifically unsound. While coconut oil may be occlusive, tea tree oil has demonstrated antimicrobial efficacy in peer-reviewed studies. The dismissal of aloe vera as purely irritating ignores its documented anti-inflammatory properties in vitro. This is not evidence-based medicine - it is dogma.
Sajith Shams December 27 2025
You think you're the first person to figure this out? I've been telling people for years that hydrocortisone is poison for the face. And now you're writing a whole article like it's news? Wake up. This is basic dermatology. Stop acting like you discovered fire.
Adrienne Dagg December 28 2025
I switched to SLS-free toothpaste and now I’m basically a new person 😌✨ no more red ring around my mouth like I’ve been crying nonstop for 3 years. also i started wearing hats and now i look like a 1920s movie star 🎩💛
Chris Davidson December 29 2025
The data presented here is statistically significant but lacks longitudinal tracking. Without controlled studies comparing outcomes across different regimens, this remains anecdotal. Also the term 'gentle' is undefined. What is gentle to one is irritating to another. This is not a protocol. It's a suggestion.
Matt Davies December 30 2025
I used to think my face was broken. Now I just think it’s been betrayed. By toothpaste. By sunscreen. By my own desperation to fix it fast. Took me 14 months. But I’m finally not hiding in photos anymore. And honestly? That’s worth every second of the flare.
Dev Sawner January 1 2026
The statistical correlations cited are misleading. Correlation does not imply causation. The prevalence of Demodex mites in the general population is 80-100% in adults. Therefore, their presence in 83% of cases is statistically insignificant. Furthermore, the 78% confidence in social impact is drawn from unvalidated self-reports. This article reads like a marketing brochure disguised as clinical guidance.
Moses Odumbe January 2 2026
bro i used hydrocortisone for a zit and now my whole face is on fire but i just found out it was perioral dermatitis?? 😵💫 i thought i was just bad at skincare. now i know it was the cream. i’m done with all that stuff. just water and hope now 🙏
bhushan telavane January 3 2026
In India, we use turmeric and neem paste for everything. I tried it here - it burned like hell. Lesson learned: what works in rural Kerala doesn’t work on a damaged facial barrier in Manhattan. This guide? Finally made sense.
Mahammad Muradov January 3 2026
The article's recommendation to avoid all makeup is impractical and culturally insensitive. Many women rely on cosmetic camouflage for professional and social stability. A blanket prohibition without acknowledging socioeconomic or psychological necessity is irresponsible.