Depression isn’t just feeling sad. It’s waking up exhausted, staring at the ceiling, and wondering why getting out of bed feels impossible. It’s losing interest in things you used to love, struggling to focus at work, or snapping at people you care about - not because you want to, but because your brain is stuck in a heavy fog. Around 280 million people worldwide live with this condition, and it’s the top cause of disability globally. The good news? We now have clear, proven ways to manage it - not just one fix, but a mix of medications, therapy, and lifestyle changes that work together.
Medications: Not a Quick Fix, But a Tool That Can Help
When doctors talk about antidepressants, they usually mean second-generation drugs like SSRIs - selective serotonin reuptake inhibitors. These include sertraline, citalopram, and fluoxetine. They’re not magic pills, but they’re the most commonly prescribed first-line options because they tend to have fewer side effects than older drugs.
Sertraline often comes up first in guidelines like NICE’s 2022 update because it’s affordable and well-tolerated. But here’s the catch: about 30-50% of people on SSRIs experience sexual side effects. That’s not rare - it’s common. SNRIs like venlafaxine can raise blood pressure in 10-15% of users. Bupropion, on the other hand, has lower sexual side effects but carries a small seizure risk - about 0.4% at standard doses.
For mild depression, guidelines like NICE say not to start medication right away. For moderate to severe cases, though, antidepressants are a solid first step. And if one doesn’t work? Don’t give up. About 30% of people need to try more than one drug before finding the right fit. It can take 4-8 weeks to see real changes, and many people quit too early.
If you’ve tried two different antidepressants and still feel stuck, that’s called treatment-resistant depression. At this point, doctors may add something like quetiapine (an atypical antipsychotic), lithium, or even thyroid hormone. Electroconvulsive therapy (ECT) is the most powerful tool for severe or psychotic depression - with remission rates of 70-90%. Yes, it can cause temporary memory issues, but for someone who can’t eat, sleep, or get out of bed, it can be life-saving.
Therapy: Talking Can Change Your Brain
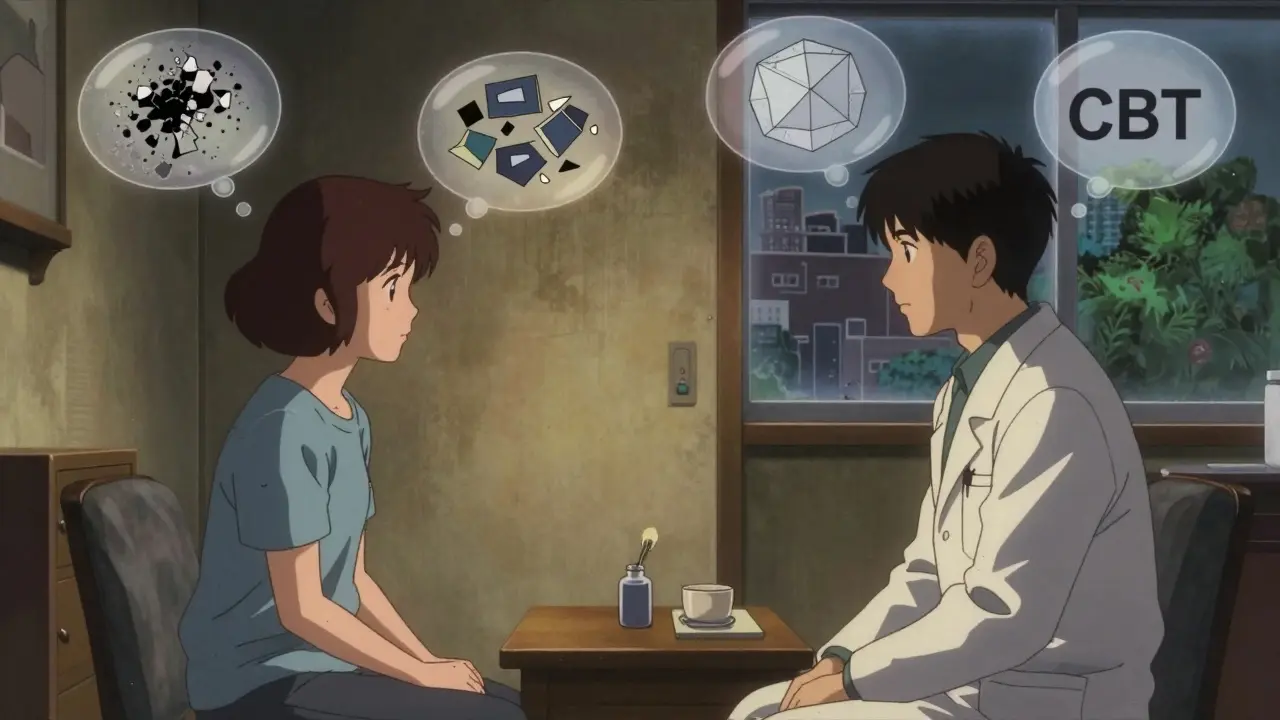
Therapy isn’t just “talking it out.” It’s structured, evidence-based work that rewires how you think and respond to stress. Cognitive Behavioral Therapy (CBT) is the gold standard. In 8-28 weekly sessions, you learn to spot negative thought patterns - like “I’m a failure” after one mistake - and replace them with more realistic ones. Studies show CBT helps 50-60% of people with mild to moderate depression.
Interpersonal Therapy (IPT) focuses on relationships. If your depression is tied to grief, conflict, or isolation, IPT can help. It typically runs 12-16 weeks and works just as well as medication for moderate cases. One 2016 meta-analysis found a 55% response rate with IPT versus 45% with no treatment.
For people who’ve had depression more than once, Mindfulness-Based Cognitive Therapy (MBCT) is a game-changer. It combines meditation with CBT techniques to prevent relapse. The 2015 PREVENT trial showed an 31% drop in relapse risk over 60 weeks compared to standard care.
And if your depression is tangled up in relationship problems? Behavioral couples therapy can help. One study showed 40-50% symptom improvement when both partners worked together - better than individual therapy alone.
Here’s what the data says: for moderate depression, CBT alone gives you a 45-50% chance of improvement. Add an antidepressant? That jumps to 55-60%. That’s why major guidelines like the American College of Physicians recommend either therapy or medication as a first step - not both, unless symptoms are severe.
Lifestyle Changes: The Hidden Powerhouse
Exercise isn’t just for your body. Three to five sessions a week of moderate activity - like brisk walking for 30-45 minutes - can match the effect of antidepressants for mild depression. A 2020 meta-analysis found a standardized mean difference of -0.68 compared to no exercise. That’s not small. That’s clinically meaningful.
Sleep matters more than you think. About 75% of people with depression have trouble sleeping. Fixing your sleep routine can cut depression severity by 30-40%. Simple rules: wake up and go to bed at the same time (within 30 minutes), only go to bed when sleepy, and stop screens an hour before bed. No scrolling, no Netflix. Just dim lights and quiet.
Diet isn’t about losing weight - it’s about brain fuel. The SMILES trial in 2017 gave people with depression a 12-week Mediterranean-style eating plan: lots of vegetables, fruits, whole grains, fish, nuts, and olive oil. The result? 32% went into remission. The control group, which got social support but no diet change? Only 8% improved.
Stress reduction techniques like mindfulness meditation (10-20 minutes daily), yoga (2-3 times a week), or tai chi (twice a week) all show moderate benefits. You don’t need to be a yogi. Just 15 minutes of progressive muscle relaxation twice a day can lower your stress hormones and ease depressive symptoms.
What Works Based on How Bad It Is
Depression isn’t one-size-fits-all. Your treatment should match your symptoms.
- Mild depression (PHQ-9 score 5-9): Skip medication unless you really want it. Try guided self-help, structured exercise, or active monitoring with your doctor. Many people improve without pills.
- Moderate depression (PHQ-9 score 10-14): Pick one: CBT or an SSRI. Both work. If you’re struggling at work or home, combine them.
- Severe depression (PHQ-9 score 15+): Start with both medication and therapy. The combo boosts response rates to 60-70%, far better than either alone.
- Psychotic depression (hallucinations, delusions): ECT or antidepressants + antipsychotics. ECT clears symptoms in 70-80% of cases.
- Chronic depression (lasting 2+ years): CBASP - Cognitive Behavioral Analysis System of Psychotherapy - is designed for this. One study showed 48% improvement with CBASP plus medication, versus 28% with meds alone.

Barriers and New Frontiers
Even with all this knowledge, only 35.6% of adults with depression in the U.S. get any treatment. There’s a shortage of therapists - over 6,000 areas are designated as mental health professional shortage zones.
Digital tools are stepping in. Apps like reSET, an FDA-cleared digital therapy, helped 47% of users in trials. But adoption is still low - only 5% of clinics use them. Telehealth changed the game, though. In 2022, 68% of providers offered virtual visits - up from 18% in 2019.
Emerging options are exciting. Psilocybin-assisted therapy showed a 71% response rate in a 2021 trial. It’s not legal yet, but research is moving fast. Meanwhile, smartphone apps that track your speech, movement, and social activity can predict a depressive episode up to seven days ahead - with 82% accuracy.
And here’s the big shift: we’re moving away from the “chemical imbalance” myth. Depression isn’t just low serotonin. It’s biology, behavior, environment, and trauma - all tangled together. That’s why personalized treatment is the future. One person needs exercise and CBT. Another needs ECT. Another needs a diet change and sleep fixes. No single path works for everyone.
What to Do Next
If you’re struggling:
- Track your symptoms with a simple PHQ-9 questionnaire (free online). It’s not a diagnosis, but it helps you talk to your doctor.
- Don’t wait for “rock bottom.” Start with one small change - a 20-minute walk three times a week, or turning off screens an hour before bed.
- Ask your doctor: “What’s the best first step for me?” Don’t assume medication is the only option.
- If therapy feels out of reach, look into online CBT programs or community mental health centers.
- Be patient. Improvement takes weeks. Relapse is common - but not inevitable.
Depression doesn’t vanish overnight. But with the right mix of tools - medication when needed, therapy that sticks, and daily habits that rebuild your energy - recovery isn’t just possible. It’s predictable. You don’t need to fix everything at once. Just start somewhere. Then keep going.
Can depression be managed without medication?
Yes, especially for mild to moderate depression. Studies show that structured exercise, cognitive behavioral therapy (CBT), improved sleep, and dietary changes like the Mediterranean diet can be as effective as antidepressants for many people. Guidelines from NICE and the American College of Physicians recommend these as first-line options for mild cases. Medication isn’t always necessary - but it can be a helpful tool when symptoms are severe or don’t improve with lifestyle and therapy alone.
How long does it take for antidepressants to work?
Most antidepressants take 4 to 8 weeks to show noticeable effects. Some people feel slight improvements in energy or sleep after 2 weeks, but full benefits usually take longer. It’s common to feel worse before you feel better, especially in the first two weeks. Don’t stop taking them unless your doctor advises it. If there’s no improvement after 8 weeks at the right dose, your doctor may adjust the medication or try a different one.
Is therapy better than medication for depression?
Neither is universally “better.” For moderate depression, CBT and SSRIs have similar effectiveness - around 50% response rates. But therapy often has longer-lasting effects. People who complete CBT are less likely to relapse after stopping treatment compared to those who stop medication. For severe depression, combining both gives the best results. The choice depends on your symptoms, preferences, and access to care.
Can exercise really help with depression?
Yes - and the evidence is strong. A 2020 meta-analysis found that 3-5 sessions per week of moderate exercise (like brisk walking) produced antidepressant effects comparable to medication for mild depression. Exercise boosts endorphins, reduces inflammation, and improves sleep - all of which help lift mood. You don’t need to run a marathon. Even 20 minutes of walking three times a week can make a measurable difference.
What if nothing seems to work?
If you’ve tried two antidepressants and therapy without relief, you have treatment-resistant depression. That’s more common than people think - about 30% of cases. Next steps include adding lithium or quetiapine to your current treatment, trying repetitive transcranial magnetic stimulation (rTMS), or considering ECT. The STAR*D trial showed that with four rounds of treatment adjustments, 67% of people eventually reached remission. Don’t give up. Finding the right combination can take time, but it’s possible.
Are there new treatments on the horizon?
Yes. Psilocybin-assisted therapy showed a 71% response rate in a 2021 trial and is under review for approval. Digital phenotyping - using smartphone data to predict depressive episodes before they happen - is already being tested with 82% accuracy. Telehealth has dramatically improved access, and digital therapeutics like reSET are FDA-cleared. While these aren’t mainstream yet, they represent a shift toward personalized, tech-enabled care that could reach more people in the next few years.

13 Comments
Jake Moore January 18 2026
Just wanted to say this post is one of the clearest summaries I’ve seen on depression management. The breakdown of meds vs therapy vs lifestyle? Spot on. I’ve been on sertraline for 6 months and it took 7 weeks to even notice a difference. Quitting at 3 weeks would’ve been a mistake. Also, the exercise stats? Real. I started walking 3x a week and my brain fog lifted faster than the meds did. Don’t underestimate movement.
Also, sleep hygiene is non-negotiable. No screens after 9? Game changer.
Joni O January 20 2026
Thank you for writing this. I’ve been stuck in depression for 3 years and this is the first time I’ve felt like someone actually gets it. I tried CBT and it felt robotic at first, but after 12 weeks I started catching my negative thoughts before they swallowed me whole. And yeah, the Mediterranean diet? I started eating more fish and nuts and my energy went from ‘crawling out of a hole’ to ‘maybe I can shower today.’ Small wins matter.
Max Sinclair January 20 2026
Really appreciate how balanced this is. Too many people treat depression like it’s either ‘just take a pill’ or ‘just get more sleep.’ It’s both and neither. The data on combo treatment for moderate cases is solid-therapy + med isn’t overkill, it’s smart. And I’m glad you mentioned ECT. So many people still think it’s 1950s horror movie stuff. It’s not. It’s science. And sometimes, it’s the only thing that pulls you back from the edge.
Nishant Sonuley January 21 2026
Man, I read this whole thing while eating a bowl of ramen at 2am because I couldn’t sleep. You know what’s wild? The part about how 75% of depressed people have sleep issues. That’s not a coincidence-that’s the system screaming. I tried melatonin, then sleep apps, then white noise machines. Nothing worked until I just… stopped trying to ‘fix’ sleep and started respecting it. No phone after 10, lights out by 11, same time every day-even on weekends. Not because it’s ‘healthy,’ but because my brain literally can’t function without rhythm. Also, I swear by walking barefoot on grass for 10 minutes. Grounding? Maybe. But I feel less like a ghost now.
And yes, psilocybin is coming. I’ve seen people come back from the dead after one session. The system’s scared of it because it can’t patent a mushroom. But hey, maybe we’re moving toward healing, not just managing.
Emma ######### January 22 2026
I’ve been on bupropion for a year. The sexual side effects were brutal at first, but they faded. What didn’t fade was the guilt I felt for even needing meds. Like I was failing at being ‘strong.’ This post reminded me: needing help doesn’t mean you’re broken. It means you’re human. And if you’re reading this and feeling alone-please know you’re not.
Andrew McLarren January 24 2026
While the empirical data presented herein is largely substantiated by peer-reviewed literature, I must express concern regarding the casual tone adopted in the exposition of clinical recommendations. The integration of colloquialisms such as ‘brain fog’ and ‘getting out of bed feels impossible’ may inadvertently diminish the perceived gravity of major depressive disorder among lay audiences. A more formal, clinically detached lexicon would better serve the educational intent of this communication.
Andrew Short January 25 2026
Let’s be real-this is all just corporate pharmaceutical propaganda wrapped in ‘science.’ SSRIs don’t fix anything. They just numb you so you can keep working for the man. The real cause? Society is broken. You’re not depressed because your serotonin’s low-you’re depressed because your life is meaningless. And now they want to drug you into compliance. Wake up. Go outside. Stop scrolling. Stop buying into the system. The pill is the problem.
christian Espinola January 25 2026
They don’t want you to know this, but antidepressants were designed by Big Pharma to keep people docile. The ‘chemical imbalance’ theory? Debunked in 2008. The FDA knew. The NIH knew. But they kept pushing it because pills = profits. And now they’re pushing ‘digital phenotyping’ and ‘psilocybin therapy’-same game, new labels. They’re not healing you. They’re monetizing your suffering. ECT? It’s not ‘life-saving.’ It’s brain damage with a side of amnesia. Read the original studies. They’re not what they claim.
Chuck Dickson January 26 2026
Yo, I was at rock bottom last year. Couldn’t get out of bed. Didn’t shower for 11 days. Tried therapy, hated it. Tried meds, felt like a zombie. Then I started walking. Just 20 minutes. Every day. No music. No podcast. Just me and the sidewalk. After 3 weeks, I noticed I was breathing deeper. After 6 weeks, I smiled at a stranger. After 3 months? I started cooking again. I didn’t need a miracle. I just needed to move. And now I tell everyone: if you’re stuck, start with your feet. Walk. Just walk. That’s it.
Naomi Keyes January 28 2026
Actually, I have to correct several inaccuracies here. First, the SMILES trial had a sample size of only 67 participants-far too small to draw population-level conclusions. Second, the claim that CBT has a 50-60% response rate? That’s misleading-it’s 50-60% improvement, not remission. And third, the assertion that ‘exercise matches antidepressants’? That’s only true in mild cases, and even then, the effect size is small and not clinically significant for most. Also, you didn’t mention the high dropout rates in behavioral interventions. People quit therapy and exercise because they’re hard. Medication is easier. That’s not a flaw-it’s a feature.
Andrew Qu January 29 2026
I’ve been a therapist for 12 years. I’ve seen people get better with meds. I’ve seen people get better with CBT. I’ve seen people get better with both. And I’ve seen people get better with nothing but time and a friend who showed up. There’s no single path. But there is one truth: recovery isn’t about fixing your brain. It’s about rebuilding your life. One small, consistent step at a time. You don’t need to be perfect. You just need to show up.
kenneth pillet January 29 2026
Exercise works. Sleep matters. Diet helps. But the real secret? Community. I didn’t get better until I started volunteering at the animal shelter. Didn’t fix my brain. But it gave me a reason to get up. And that’s more powerful than any pill.
Also, typos are fine. We’re all just trying.
Danny Gray January 29 2026
Interesting how we treat depression like a puzzle to be solved, when maybe it’s not a problem to fix at all. Maybe it’s a signal. A deep, quiet voice saying: ‘Your life doesn’t match your soul.’ We rush to medicate, to ‘optimize,’ to ‘manage’-but what if the answer isn’t in a pill or a therapy app? What if the answer is to stop running? To sit with the silence? To quit the job, leave the city, burn the spreadsheet? We’ve turned healing into a productivity hack. Maybe depression isn’t the enemy. Maybe it’s the last honest thing left in a world that’s lost its way.