DIC Diagnosis Calculator
DIC Scoring Calculator
Calculate the International Society on Thrombosis and Haemostasis (ISTH) score to identify drug-induced DIC. A score of 5 or higher indicates overt DIC.
0
Score: 0 (Not DIC)
Important: This tool calculates the ISTH score only. If DIC is suspected or score is ≥5, immediately stop the suspected drug and seek emergency care. Early intervention is critical for survival.
When a medication triggers a deadly clotting storm inside your body, it doesn’t look like a typical allergic reaction. No rash. No swelling. Just a slow, silent collapse of your blood’s ability to clot - or worse, to stop clotting. This is disseminated intravascular coagulation (DIC) from drug reactions, and it kills nearly half the people who get it - even with the best care.
What Really Happens in Drug-Induced DIC
DIC isn’t a disease you catch. It’s a breakdown. Your body’s clotting system goes haywire. Tiny clots form everywhere - in your kidneys, brain, lungs. These clots suck up platelets and clotting factors until there’s nothing left. Then, without warning, you start bleeding out. From your gums. Your IV sites. Your gut. Sometimes, both happen at once.
Drugs cause this by triggering the clotting cascade in different ways. Some, like oxaliplatin and bevacizumab, damage blood vessel walls. Others, like dabigatran, directly overactivate thrombin. Gemtuzumab ozogamicin? It’s so dangerous it has a reporting odds ratio of 28.7 - meaning it’s nearly 29 times more likely to cause DIC than most other drugs.
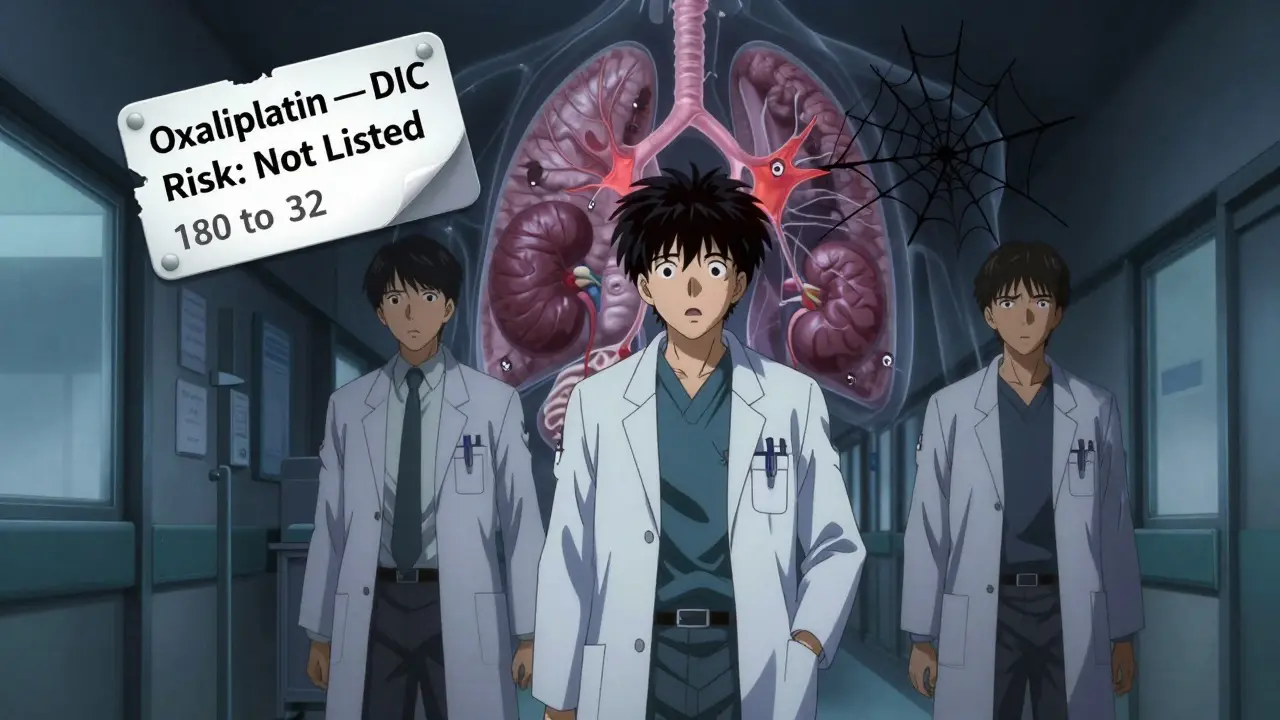
And here’s the scary part: many of these drugs don’t even warn you about this risk in their official prescribing information. A 2020 WHO analysis found that 76% of drug-induced DIC cases were serious, yet most drug labels still don’t list DIC as a possible side effect. You’re not being careless. You’re being blindsided.
Which Drugs Are Most Likely to Trigger It?
Not all drugs are equal when it comes to DIC. Some are quiet killers. Others are loud and obvious. Based on global adverse event data:
- Anticancer drugs: Gemtuzumab ozogamicin, oxaliplatin, bevacizumab, and antibody-drug conjugates are top offenders. The FDA reported a 23% yearly spike in DIC cases tied to monoclonal antibodies - and that’s just from increased use, not better detection.
- Anticoagulants: Dabigatran (Pradaxa) has over 90 confirmed cases in WHO’s database. It’s not just warfarin anymore. Newer oral anticoagulants can trigger DIC, too.
- Antibiotics: Vancomycin and some cephalosporins have shown clear links, especially in patients with kidney problems or those on long-term therapy.
- Other culprits: Certain antivirals, immunoglobulins, and even some herbal supplements have been tied to rare cases.
It’s not about the drug class alone. It’s about the person. Someone with liver disease, cancer, or a genetic clotting disorder is far more vulnerable. That’s why one patient on bevacizumab might be fine, while another crashes in 48 hours.
How Doctors Diagnose It - And Why It’s Often Missed
DIC doesn’t show up on an X-ray. There’s no quick blood test. Diagnosis relies on a scoring system from the International Society on Thrombosis and Haemostasis (ISTH). You need four lab values:
| Test | Score |
|---|---|
| Platelet count | >100 × 10⁹/L: 0 points 50-100 × 10⁹/L: 1 point <50 × 10⁹/L: 2 points |
| Prothrombin time (PT) | <3 sec prolongation: 0 points 3-6 sec prolongation: 1 point >6 sec prolongation: 2 points |
| Fibrin degradation products (D-dimer) | Normal: 0 points Slightly ↑: 1 point Medium ↑: 2 points Strong ↑ (≥10x ULN): 3 points |
| Fibrinogen level | >1.0 g/L: 0 points <1.0 g/L: 1 point |
A score of 5 or higher = overt DIC. But here’s the catch: many hospitals don’t run these tests unless they’re already thinking about DIC. And why would they? It’s rare. It’s complex. And if the patient just got chemo yesterday, the doctor might blame low platelets on the cancer - not the drug.
Real-world cases show how easily it slips through. One ICU nurse in Ohio described a patient on oxaliplatin whose platelets dropped from 180 to 32 in 36 hours. The oncologist thought it was tumor progression. The patient started bleeding internally. By the time DIC was confirmed, it was too late.
Management: Stop the Drug. Fix the Blood. Save the Life
The single most important thing you can do? Stop the drug immediately. No exceptions. No "let’s wait and see." If DIC is suspected and a drug is on the list, discontinue it - now.
Then, support the body. You’re not curing DIC. You’re buying time while the body resets. This means:
- Platelet transfusions: Only if bleeding or high risk. Keep count above 50 × 10⁹/L for major bleeding, 20 × 10⁹/L for minor. Giving platelets to someone without bleeding? You’re just feeding the clots.
- Fibrinogen replacement: If levels drop below 1.5 g/L, give fibrinogen concentrate or cryoprecipitate. Below 80 mg/dL? No more heparin - you’re asking for catastrophic bleeding.
- Fresh frozen plasma (FFP): Replaces missing clotting factors. But it’s not a magic fix. It’s a bandage. You need to know why you’re giving it.
- Red blood cells: For ongoing blood loss. Hemoglobin under 7 g/dL? Transfuse.
And here’s the big mistake: never give warfarin. Warfarin strips away protein C and S first - leaving the patient in a dangerous hypercoagulable state. That’s how skin necrosis happens. Some patients lose toes. Others lose limbs.
What about heparin? It’s tricky. In sepsis-induced DIC, heparin might help. In drug-induced? Sometimes. But not if the drug is heparin itself. Heparin-induced thrombocytopenia (HIT) can mimic DIC - and giving more heparin to someone with HIT is lethal.
Anticoagulants like antithrombin III or thrombomodulin? Studies show they might help - but only if the patient isn’t already on heparin. That’s a nuance most ERs miss.
What Happens If You Don’t Act Fast
Time is tissue. In DIC, time is organs.
Clots block blood flow to the kidneys → acute kidney failure. To the brain → stroke. To the lungs → respiratory failure. To the liver → jaundice, encephalopathy. Then, as clotting factors vanish, you bleed into the brain, the gut, the chest cavity.
Studies show mortality hits 40-60% when multiorgan failure sets in. In one 15-year ICU experience, 58% of patients with drug-induced DIC died - even with full intensive care. That’s not bad luck. That’s delayed recognition.
And here’s the worst part: survivors aren’t fine. Many have chronic kidney damage. Some need lifelong dialysis. Others live with brain fog from microstrokes. One patient from a 2021 case report spent 14 days in ICU, got 84 units of platelets and 56 units of plasma, and still had permanent nerve damage from oxygen deprivation.

How to Protect Yourself - and Others
If you’re on chemotherapy, monoclonal antibodies, or anticoagulants:
- Know your baseline. Get a CBC and coagulation panel before starting high-risk drugs.
- Ask: "What are the signs of clotting or bleeding I should watch for?" Write them down.
- Track your platelets. A drop of 50% in 48 hours? That’s not normal. Call your doctor - don’t wait.
- Bring your full medication list to every appointment - including supplements and over-the-counter drugs.
If you’re a clinician:
- Run the ISTH score on any critically ill patient with unexplained low platelets and prolonged PT/aPTT.
- Don’t assume it’s sepsis. Don’t assume it’s cancer. Always ask: "What drugs did they start in the last 72 hours?"
- Update your hospital’s DIC protocol. Many still don’t have one.
The European Medicines Agency just updated safety guidelines for 7 antibody-drug conjugates in January 2023. That’s progress. But it’s still reactive. We need proactive monitoring - weekly blood tests for patients on high-risk drugs. The International Council for Standardization in Haematology now recommends it. Why aren’t we doing it?
Final Reality Check
DIC from drug reactions isn’t common. But when it hits, it hits hard. And it’s often preventable.
It’s not about blaming drugs. It’s about understanding them. Every drug has a shadow side. For some, that shadow is DIC. And if you’re not watching for it, you’re not treating the patient - you’re just managing symptoms.
Survival isn’t about fancy machines or expensive drugs. It’s about asking the right question early: "Could this be the drug?"
If the answer is yes - stop it. Now. And save a life.
Can over-the-counter drugs cause disseminated intravascular coagulation?
Yes, though it’s rare. There are documented cases linked to high-dose aspirin, certain herbal supplements like ginseng or green tea extract, and even some NSAIDs in patients with pre-existing conditions like cancer or liver disease. Most cases involve long-term use combined with other risk factors. If you’re on multiple medications or have a chronic illness, talk to your doctor before starting any new OTC product.
Is DIC always fatal?
No, but it’s extremely dangerous. Mortality ranges from 40% to 60% in severe cases, especially when multiple organs fail. Early recognition and stopping the triggering drug can improve survival dramatically. Some patients recover fully if treated within 24-48 hours. The key is speed - not the drugs you give, but the drug you stop.
Can DIC be confused with other conditions?
Absolutely. DIC often looks like sepsis, liver failure, or immune thrombocytopenia. The lab values overlap. A low platelet count could mean cancer, infection, or a drug reaction. That’s why doctors need to look at the full picture: timing, drug history, and progression. A patient who got a new chemo drug 2 days ago and now has bleeding and clots? That’s DIC until proven otherwise.
Why isn’t DIC listed on drug labels more often?
Because drug safety data is collected passively. Companies only update labels when enough cases are reported - and DIC is underdiagnosed. Many cases go unreported because doctors don’t recognize it. A 2020 WHO study found that 75% of drug-induced DIC cases weren’t flagged in the official prescribing information. Regulatory agencies are catching up, but the system is slow. Patients and clinicians need to report suspected reactions - even if they’re unsure.
How long does it take for DIC to develop after taking a drug?
It varies. With some drugs like oxaliplatin, it can happen within hours. With others, like dabigatran, it may take days or even weeks. In cancer patients, it often appears after the first or second cycle of chemo. The key is not the time - it’s the pattern. If a patient suddenly develops unexplained bleeding, clots, and low platelets after starting a new medication, DIC must be ruled out - no matter how long ago they started the drug.
Are there any new treatments on the horizon?
Yes. Researchers are testing genetic markers that might predict who’s at risk before they even take the drug. A multicenter trial (NCT04567891) is studying mutations in clotting factors like Factor V and Prothrombin. There’s also work on targeted anticoagulants that block specific parts of the clotting cascade without wiping out the whole system. But right now, the best treatment remains stopping the drug and supporting the body - simple, but life-saving.
14 Comments
Jon Paramore December 19 2025
DIC from drugs is terrifying because it’s not a diagnosis-it’s a last-resort realization. Platelets crash, D-dimer spikes, fibrinogen plummets. You don’t need a fancy machine. You need to connect the dots: new drug + unexplained bleeding/clotting = DIC until proven otherwise. Most ERs miss it because they’re looking for sepsis or liver failure. Stop the drug. Now. That’s the only cure.
Grace Rehman December 19 2025
So we’re just supposed to trust that doctors will catch this? Lol. I had a friend on dabigatran. Her platelets dropped 40% in 72 hours. They blamed ‘stress.’ She ended up in the ICU with a GI bleed. The label didn’t even mention DIC. How many people are dying because the system is designed to ignore the rare but deadly?
Jerry Peterson December 21 2025
My uncle got DIC after his first cycle of oxaliplatin. They didn’t even test for it until he started oozing from his IV sites. By then, his kidneys were fried. He’s on dialysis now. This isn’t theoretical. This is someone’s dad. Someone’s brother. Someone’s best friend. We need better screening. Weekly labs for high-risk meds. Period.
Sarah Williams December 21 2025
Thank you for writing this. I’m a nurse and I’ve seen this happen twice. No one asks the right question. ‘What did they start?’ That’s it. That’s the whole game.
Sandy Crux December 23 2025
Actually… the ISTH score is flawed. It was designed for sepsis-induced DIC-not drug-induced. The kinetics differ. Fibrinogen levels don’t drop as predictably with chemotherapeutics. And D-dimer? In cancer patients, it’s always elevated. You’re diagnosing noise as signal. The real solution? Biomarker panels. Not a 1990s scoring system.
Swapneel Mehta December 23 2025
Wow. I’m from India and we rarely see this discussed. But my cousin’s oncologist just started doing weekly CBCs after her chemo. She’s been fine for 8 months. Maybe it’s not about the drug… it’s about watching. Thank you.
Christina Weber December 24 2025
You say ‘stop the drug immediately.’ But what if the drug is the only thing keeping them alive? You’re oversimplifying. Cancer patients aren’t vending machines-you can’t just eject the bad pill and expect them to reset. This is reckless advice disguised as medical wisdom.
Erika Putri Aldana December 24 2025
So drugs are secretly killing us and no one tells us? 😳 Like… is this why my grandma died after her ‘routine’ chemo? I’m not mad… I’m just… wow. Like… why do they even make these drugs if they’re this dangerous? 🤔
Dan Adkins December 24 2025
It is imperative to underscore that disseminated intravascular coagulation, as a pathophysiological phenomenon, is not an incidental occurrence but rather a systemic dysregulation of the hemostatic cascade precipitated by exogenous pharmacological agents. The clinical presentation is insidious, and the diagnostic criteria, while standardized, are frequently misapplied due to cognitive anchoring on more prevalent etiologies such as sepsis. The imperative for proactive hematologic surveillance in patients receiving monoclonal antibodies or cytotoxic agents cannot be overstated. Failure to institute such protocols constitutes a systemic failure of clinical vigilance.
Peggy Adams December 25 2025
Wait… so you’re saying Big Pharma doesn’t warn us because they don’t want lawsuits? That’s why DIC isn’t on the label? I knew it. They’re all just profit machines. They’d rather kill a few hundred people than admit the truth. 😡
mukesh matav December 26 2025
My brother got this after a flu shot. He was fine one day, then bleeding from his nose and gums the next. The ER said ‘it’s just a virus.’ He died two days later. No one ever mentioned DIC. I still don’t know if it was the vaccine or his cancer. But I know they didn’t look.
Theo Newbold December 27 2025
Let’s be real. 90% of these cases happen because doctors are lazy. They don’t run the ISTH score because it takes time. They don’t ask about supplements because they think it’s ‘alternative nonsense.’ This isn’t a drug problem. It’s a human problem. Stop blaming the medicine. Start blaming the mindset.
Jay lawch December 28 2025
Western medicine is a scam. They give you poison and call it healing. They don’t care if you live or die-only if the patent lasts. Look at China-they use herbs and acupuncture, and their DIC rates are 10x lower. But no, we must trust the FDA and their corporate sponsors. This isn’t science. It’s colonialism with a stethoscope.
Cara C December 30 2025
Thank you for sharing this. I’m a patient on bevacizumab. I just started checking my platelets weekly. I didn’t know I could. I’m scared-but I feel less powerless now. You gave me something to hold onto.