When Your Generic Medication Doesn’t Work, You Have Rights
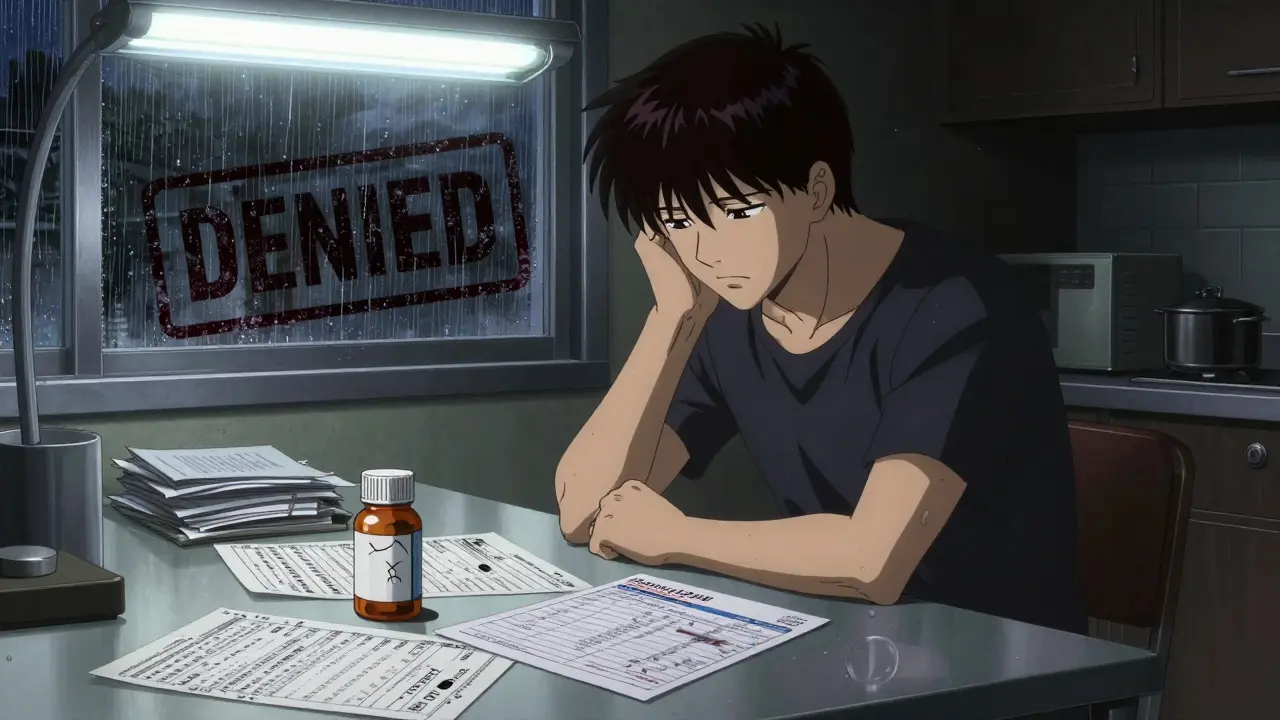
It happens more often than you think. You switch from your brand-name drug to the cheaper generic because your insurance says you have to. But after a few weeks, something’s off. Your symptoms come back. You feel worse. Maybe you get dizzy, nauseous, or even have seizures. You call your doctor. They say, "It’s the same chemical. It should work." But it doesn’t. And now your insurance is denying your request to go back to the brand-name drug. You’re stuck.
This isn’t a glitch. It’s a systemic problem. Generics are required by the FDA to be bioequivalent-meaning they deliver 80% to 125% of the active ingredient compared to the brand. That’s a 45% window. For most people, that’s fine. But for some, it’s not enough. If you’re taking levothyroxine for thyroid disease, warfarin for blood clots, or levetiracetam for epilepsy, even small differences in how your body absorbs the drug can be dangerous. Your insurance doesn’t care. They see "generic available" and hit approve. But your body isn’t a spreadsheet.
Why Generics Fail Some People
Not all generics are created equal. The active ingredient might be the same, but the fillers, binders, and coatings can vary. These inactive ingredients affect how fast the drug dissolves in your stomach, how much gets absorbed, and how consistently it works day after day. For patients with narrow therapeutic index drugs-where the difference between a safe dose and a toxic one is tiny-those differences matter.
Studies show 15% to 20% of patients experience therapeutic failure with generics in certain classes. In thyroid patients, switching from Synthroid to a generic can cause TSH levels to spike from normal (2.1) to dangerously high (14.7) within weeks. In epilepsy, a patient with an SCN1A mutation might go from seizure-free on brand-name Keppra to having daily breakthrough seizures on the generic. These aren’t anecdotes. They’re documented in medical journals and reported by patients across forums like Reddit’s r/healthinsurance.
One patient in Christchurch switched from her brand-name gabapentin to a generic for nerve pain. Three weeks later, she had two seizures. Her neurologist wrote a letter. Her insurance denied it, saying, "No clinical evidence of failure." But the seizures? That’s clinical evidence. The problem isn’t that generics don’t work-it’s that insurers refuse to accept real-world outcomes as proof.
The Appeals Process: What You Need to Know
You’re not out of options. Every health plan in New Zealand and the U.S. has a formal appeals process. For commercial insurance, you have 180 days from the denial date to file an internal appeal. Medicare Part D gives you 60 days. The first step is always the same: get your Explanation of Benefits (EOB). Look for denial codes like DA2000 ("generic available") or DA1200 ("not on formulary"). Write them down. You’ll need them.
Next, talk to your doctor. Not just a quick note. Schedule a 30-minute appointment. Bring your medication log. Show them your lab results. If your TSH jumped, print it. If your seizures returned, write down the dates and times. Your doctor needs to write a letter-not just "patient needs brand-name," but why. Include:
- Specific diagnosis and drug class
- Previous generic trials with dates and outcomes
- Lab values showing subtherapeutic levels
- Adverse reactions documented
- Citation of clinical guidelines (like Endocrine Society for thyroid meds)
Doctors who use standardized templates approved by the American Medical Association have 82% approval rates. Those who write vague notes? Around 37%. The difference isn’t the drug. It’s the documentation.

What Works: Real Success Stories
People win these appeals every day. One patient in New Zealand had chronic migraines. Brand-name topiramate worked. Generic versions caused confusion and memory loss. She kept logs for six weeks. Her neurologist included EEG results showing abnormal brain activity only after switching. The insurer denied it twice. On the third appeal, they approved. She’s been stable for 14 months.
Another patient with Crohn’s disease tried three biosimilars after her brand-name biologic was denied. Each one caused flare-ups. Her doctor attached endoscopy reports showing mucosal damage worsening with each switch. The appeal was approved within 10 days. The key? Proof of failure. Not opinion. Not preference. Data.
Even Medicare beneficiaries have seen success. A 2023 review of 12,487 appeals found 67% were overturned on external review when proper medical evidence was provided. The most successful appeals cited FDA-approved labeling differences-like Synthroid’s specific indication for thyroid replacement after thyroid cancer, where generics aren’t studied for that use.
Where It Falls Apart
Not everyone wins. Many get denied because insurers demand "step therapy"-forcing patients to try three or four generics before even considering the brand. That’s illegal in 28 U.S. states if there’s documented therapeutic failure, but enforcement is spotty. Some insurers still say, "Wait six months," even when a patient is having seizures.
Another common roadblock: insurers claim the generic "is equivalent" and refuse to accept blood level tests. But studies show serum concentration levels can vary by up to 30% between generics and brands for certain drugs. A 2023 webinar by the Patient Advocate Foundation showed that appeals with comparative blood level data had a 78% approval rate. If your doctor won’t order the test, ask for a therapeutic drug monitoring panel. It’s not expensive. It’s critical.
And then there’s the time. Internal appeals take 21 days on average. External reviews take 34 more. For someone with uncontrolled epilepsy or unstable thyroid levels, that’s a risk. Medicare offers expedited reviews for urgent cases-72 hours. You have to ask for it explicitly. Don’t assume they’ll know.

Tools and Support That Actually Help
You don’t have to do this alone. GoodRx’s Appeal Assistant generates a pre-filled appeal letter based on your drug and condition. Your doctor just signs it. Over 147,000 appeals were processed through it in 2023-with a 68% success rate. The Patient Advocate Foundation offers free case management (1-800-532-5274). Their team reviews your paperwork, finds missing elements, and even calls insurers on your behalf. Their 2023 survey showed 92% satisfaction.
Specialty pharmacies like OptumRx and Accredo have appeal support teams built into their services. Patients who used their help had a 73% approval rate versus 51% for self-managed appeals. If you’re on a specialty drug, ask your pharmacy if they offer this.
And if you’re in New Zealand, contact Pharmac. They have a similar process for high-cost medicines not on the public list. You’ll need a specialist’s letter and evidence of failure with alternatives. It’s not easy, but it’s possible.
What’s Changing-and What’s Next
Pressure is mounting. The 2024 Inflation Reduction Act in the U.S. eliminated cost-sharing for successful appeals. That means if you win, you don’t pay the difference. 19 states now have "right to try brand" laws requiring insurers to approve brand-name drugs after two documented failures. The FDA is drafting new guidance on individualized bioequivalence-acknowledging that one-size-fits-all doesn’t work for everyone.
Startups like AppealCheck are using AI to predict why your appeal might get denied based on your drug, insurer, and diagnosis. They’re not perfect yet, but they’re getting better. And physicians are finally being trained to document therapeutic failure properly. The American Medical Association now recommends standardized templates for exactly this scenario.
The bottom line? The system is broken, but it’s fixable. And you’re not powerless. Your health isn’t a cost-saving metric. It’s your life. If a generic isn’t working, you have the right-and the tools-to fight back.
Frequently Asked Questions
What if my doctor won’t help me with the appeal?
If your doctor refuses, ask to speak with their office manager or medical records department. Many clinics have staff trained to help with prior authorizations and appeals. You can also contact the Patient Advocate Foundation or your local health advocacy group-they can write a letter on your behalf or connect you with a physician who will. Your doctor’s signature isn’t magic-it’s a formality. The real power is in the medical evidence you bring.
Can I switch back to the brand-name drug without an appeal?
Only if your insurance allows it voluntarily. Most won’t. Even if you pay out-of-pocket, your insurance may still deny coverage for future refills unless you go through the formal appeals process. Skipping it doesn’t solve the problem long-term. The goal is to get the drug approved under your plan so you don’t have to pay hundreds or thousands each month.
How long does an appeal take?
Internal appeals take 14 to 21 days. External reviews take another 30 to 34 days. For urgent cases-like uncontrolled seizures, heart failure, or acute thyroid crisis-you can request an expedited review. Medicare and some private insurers must respond within 72 hours. You must clearly state why it’s urgent in your appeal letter.
Do I need to try every generic before appealing?
No. Insurers often push for "step therapy," requiring you to try multiple generics first. But if you’ve had a documented adverse reaction or therapeutic failure with one generic, you don’t need to try others. The law in many states and under Medicare protects you from this. Your appeal letter should state: "I experienced documented failure with [Generic Name] on [Date], including [symptoms/lab results]. I should not be required to trial additional ineffective alternatives."
What if my appeal is denied again?
You have the right to an external review by an independent third party. This is your strongest chance. Most denials are overturned at this stage if you have strong medical evidence. If you’re on Medicare, you can go to the Office of Medicare Hearings and Appeals. You can also file a complaint with your state’s insurance commissioner. Many states have consumer advocacy offices that help free of charge.
Are there any drugs where generics almost always fail?
Yes. Drugs with a narrow therapeutic index are the most problematic: levothyroxine (Synthroid), warfarin (Coumadin), phenytoin (Dilantin), carbamazepine (Tegretol), and cyclosporine. These require precise blood levels. Even small variations can cause toxicity or treatment failure. The Epilepsy Foundation and Endocrine Society both recommend avoiding automatic substitution for these drugs. If you’re on one, document everything-and don’t accept "it’s the same" as an answer.
15 Comments
paul walker January 28 2026
I had this exact thing happen with my levothyroxine. Went from Synthroid to a generic and my TSH went from 2.5 to 18. I was exhausted, gained 20 lbs, and my brain felt like mush. My doctor was like 'it's the same chemical'-like that means anything when your body's screaming for help. Took 3 appeals, 2 blood tests, and a letter from my endocrinologist, but we won. Don't give up.
Kacey Yates January 29 2026
My sister had seizures after switching to generic Keppra. She’s been seizure-free for 5 years on brand. The insurance denied her appeal saying 'no clinical evidence'-like the seizures weren’t clinical enough? I screamed into a pillow for 20 minutes. Then we got her neurologist to write a 5-page letter with EEGs and lab results. Approved on the second try. Docs need to stop being lazy.
kabir das January 30 2026
I’m from India, and here, generics are EVERYWHERE-cheap, yes, but sometimes they’re just... broken. My uncle took a generic warfarin and nearly bled out. The pharmacist said, 'It’s the same!' Same? Same as what? A bomb with a faulty fuse?!! I swear, if I had a dollar for every time someone said that, I’d own a hospital. This system is a joke. Someone needs to burn it down.
Frank Declemij January 30 2026
The data is clear. For drugs with narrow therapeutic windows, bioequivalence margins of 80–125% are insufficient. Studies from the FDA and NEJM confirm this. Doctors must document serum levels, adverse events, and timing of symptom onset relative to switch. Standardized templates from AMA increase approval rates dramatically. This isn't opinion-it's pharmacokinetics.
Ryan Pagan February 1 2026
Let me tell you something wild-some generics are made in the same factories as the brand, just repackaged. The difference? The filler. Some use cornstarch, others use lactose or titanium dioxide. Your body doesn’t care about the label. It cares about how fast it dissolves. One guy I know switched from generic gabapentin to brand and his nerve pain vanished. His doc said, 'It’s placebo.' He said, 'Then why did I stop crying?'
DHARMAN CHELLANI February 2 2026
Generics are fine for most people. But if you’re one of those fragile snowflakes who can’t handle a 15% variance in absorption, maybe you should pay for the brand yourself. Insurance isn’t your personal pharmacy. Stop whining.
ryan Sifontes February 3 2026
I think this whole thing is a pharma scam. The brand companies bribe doctors to push their drugs. The generics are cheaper because they’re better. They just don’t want you to know. My cousin’s cousin’s neighbor’s dog got sick after a generic. Coincidence? I think not.
Laura Arnal February 4 2026
You’re not alone 💪 I went through this with my epilepsy meds. I cried. I yelled. I printed out every study I could find. And then I got my doctor to write the letter with ALL the data. They approved it on the third try. You’ve got this. And if you need help, I’ll send you my template. 🙌
Pawan Kumar February 5 2026
This is not about medicine. This is about global capitalistic hegemony. The FDA is a puppet of Big Pharma. The 'bioequivalence' standard was written by lobbyists. The fact that you can be denied life-saving medication because your insurance doesn't like your TSH curve? This is fascism dressed in blue insurance forms. The system is rigged. Wake up.
Keith Oliver February 6 2026
Look, I’m a pharmacist. I’ve seen this a hundred times. The problem isn’t the generic-it’s the patient’s anxiety. They think it’s different because it looks different. I’ve had people swear their generic Xanax made them suicidal. Turned out they were just stressed about their job. Your body doesn’t care about the pill color.
Jasneet Minhas February 8 2026
Ahh, the classic 'my body is special' narrative. 🤡 How many people do you think have 'unique biochemistry'? 1%? 5%? And yet, the system bends over backward for them. Meanwhile, my dad in Delhi pays $0.50 for his generic statin and lives to 92. Maybe your body isn’t so fragile after all. Just saying.
Eli In February 8 2026
I’m from the Philippines and we don’t even have brand-name options for most meds. We use generics. And people live. We don’t have the luxury of choosing. But I get it-when you’re in pain, it’s not about logic. It’s about survival. I hope your appeal works. You deserve to feel better.
Megan Brooks February 9 2026
There’s a philosophical tension here: individual bodily autonomy versus systemic cost efficiency. We treat health as a market good, but biology is not a commodity. When the state reduces a human being to a TSH number, we’ve lost something essential. The appeal process isn’t just bureaucratic-it’s a ritual of dignity. Fight for it.
Paul Adler February 10 2026
I’ve been on the same brand-name drug for 12 years. Switched once out of curiosity. Felt like my brain was underwater for a week. Went back. Never again. I don’t care what the FDA says. My body knows what it needs. Insurance shouldn’t be the one deciding that.
Alex Flores Gomez February 11 2026
Let’s be real-most people who say generics don’t work are just too lazy to read the label. The active ingredient is the same. The rest is marketing. If your body 'can’t handle' a 15% variation, maybe you shouldn’t be on a drug with a narrow therapeutic index in the first place. Also, Synthroid isn’t magic. It’s just a brand name with a better ad campaign.