Opioid Dosing Calculator for Older Adults
Safe Opioid Starting Dose Calculator
Calculate adjusted opioid doses for patients 65+ based on geriatric guidelines. Inputs account for age-related changes and renal function.
Results
Recommended Starting Dose:
Fall Risk Level:
Delirium Risk Level:
Key considerations: Always monitor for drowsiness, unsteadiness, or confusion within 24-48 hours. Consider non-opioid alternatives for chronic pain.
High-risk note: Patients with moderate/severe renal impairment should avoid tramadol due to increased delirium risk.
Older adults are more likely to be prescribed opioids than ever before-and more likely to suffer serious harm from them. While these drugs can ease pain, they also raise the risk of falls, confusion, hospital stays, and even death in people over 65. The problem isn’t just overprescribing. It’s that doctors often use the same dosing rules for seniors as they do for younger patients, even though aging changes how the body handles drugs. This mismatch puts older adults in danger, especially those with dementia, mobility issues, or multiple chronic conditions.
Why Opioids Are Riskier for Older Adults
As we age, our bodies change in ways that make opioids more dangerous. Kidneys and liver don’t clear drugs as quickly. Body fat increases while muscle mass drops, so opioids build up in the system longer. The blood-brain barrier becomes more porous, letting more of the drug reach the brain. These changes mean a dose that’s safe for a 40-year-old could be toxic for a 75-year-old. A 2011 study found that, on average, 80 adults aged 65 and older visited emergency rooms every day because of problems with narcotic pain relievers. Seven of those visits involved heroin. That’s not just misuse-it’s often a result of unintended side effects from prescribed medication. Emergency visits for opioid issues in this age group jumped 112% between 2005 and 2014. Inpatient stays rose by 85% in the same period.Falls: A Silent Epidemic
Falls are the leading cause of injury-related death in older adults. Opioids make them far more likely. The drugs cause drowsiness, dizziness, low blood pressure when standing up, and slowed reaction times. Even weak opioids like tramadol increase fall risk-not just from sedation, but by triggering hyponatremia, a drop in sodium levels that causes confusion and unsteadiness. One study of 2,341 adults over 60 found that those taking opioids had a 6% fracture rate over 33 months, compared to 4% for those not on opioids. While the difference wasn’t statistically significant, the trend is clear: opioids impair balance. And for someone who’s already at risk for falls, even a small increase in dizziness can mean a broken hip-and a lifetime of disability.Delirium: When Pain Medication Causes Confusion
Delirium is sudden, severe confusion. It’s often mistaken for dementia or depression, especially in older adults. But opioids are a major trigger. A 2023 study from the Danish Dementia Research Centre tracked 75,471 people over 65 with dementia. Of those, 31,619 were prescribed opioids. The results were alarming: those who started opioids had an elevenfold higher risk of dying in the first two weeks compared to those who didn’t. This isn’t about addiction. It’s about brain chemistry. Opioids interfere with neurotransmitters that control attention, memory, and awareness. In someone with existing cognitive decline, even a low dose can push them into delirium. Many doctors don’t connect the dots. They see confusion and assume it’s just dementia getting worse. But sometimes, it’s the medication.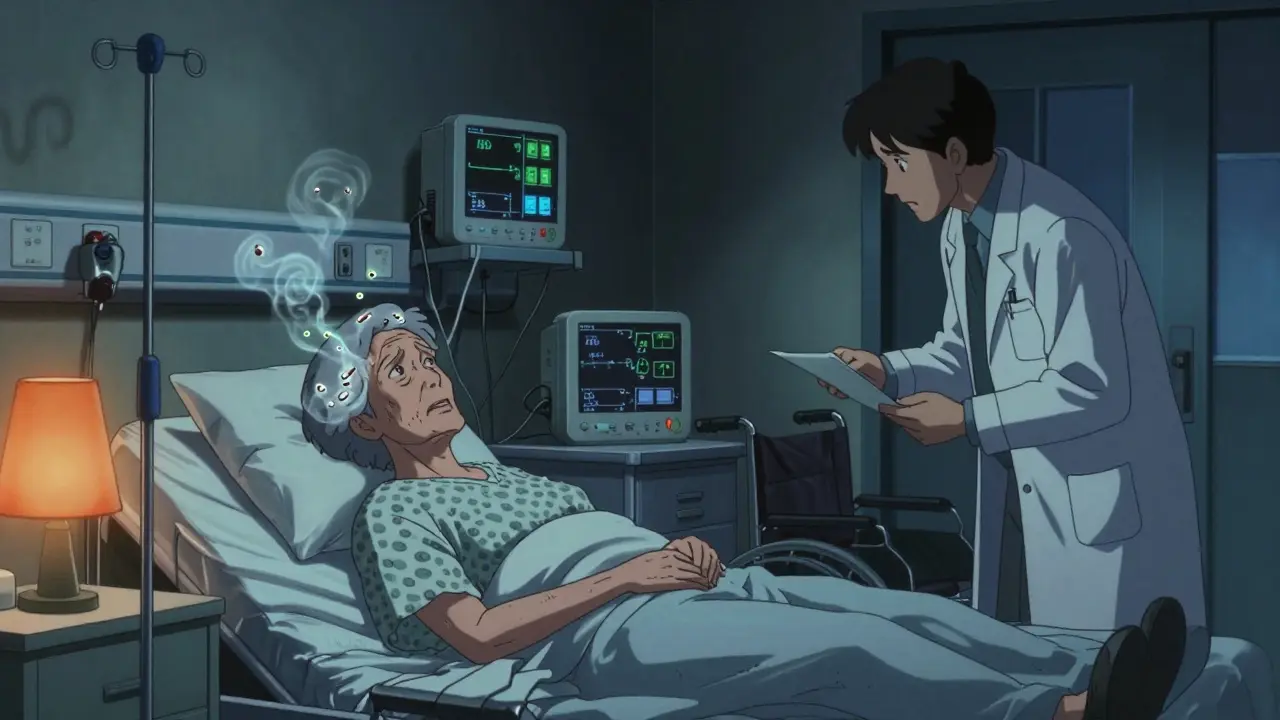
Dose Adjustments: Start Low, Go Slow
There’s no one-size-fits-all dose for older adults. The standard advice is simple: start low, go slow. That means beginning with 25% to 50% of the dose you’d give a younger adult. For example, if a typical starting dose for a 40-year-old is 10 mg of oxycodone every 6 hours, a 75-year-old might start with 2.5 mg every 8 hours. Monitoring is just as important as the starting dose. Doctors should check for signs of sedation, unsteadiness, or mental fog within days of starting or changing the dose. If the patient seems drowsy, confused, or has trouble walking, the dose should be lowered-or stopped. Tools like STOPPFall help clinicians decide when to reduce or stop opioids in people who’ve already fallen or are at risk. It’s not about denying pain relief. It’s about finding safer ways to manage it.Drug Interactions: The Hidden Danger
Most older adults take multiple medications. Opioids don’t exist in a vacuum. They interact dangerously with benzodiazepines (like Xanax), sleep aids, antidepressants, and even some heart medications. These combinations amplify sedation and respiratory depression. Tramadol is especially risky because it’s metabolized by two liver enzymes-CYP2D6 and CYP3A4. Many common drugs block these enzymes, causing tramadol to build up to toxic levels. A patient on tramadol and an SSRI antidepressant might not realize their confusion and falls are drug-induced. A 2019 study of 297,314 patients found that those who took opioids for 180 days or more over 3.5 years had more than double the risk of heart attack. Another study of over 11,000 people showed a 28% higher chance of heart attack while actively using opioids. The link isn’t fully understood, but it’s real-and it’s another reason to avoid long-term use.

12 Comments
Rachel Cericola December 24 2025
Let me tell you something important: we're not just talking about pain management here-we're talking about dignity. Older adults aren't broken machines that need a chemical fix. They're people who've lived full lives, and their bodies have earned respect, not a one-size-fits-all opioid script. The data is crystal clear: even low-dose tramadol can trigger hyponatremia, which leads to falls, which leads to hip fractures, which leads to nursing homes and isolation. We need to stop normalizing this. Start low, go slow isn't a suggestion-it's a moral obligation. And if your EHR doesn't have STOPPFall alerts built in, you're doing harm by omission.
niharika hardikar December 25 2025
The pharmacokinetic alterations in geriatric populations necessitate a paradigm shift in opioid prescribing protocols. Hepatic clearance is diminished by approximately 30% after age 65, while volume of distribution increases due to elevated adipose tissue and reduced lean body mass. Furthermore, the blood-brain barrier exhibits increased permeability, resulting in amplified CNS drug exposure. Consequently, standard adult dosing regimens constitute a iatrogenic hazard. Adherence to Beers Criteria and STOPPFall algorithms is not optional-it is a standard of care.
Blow Job December 25 2025
I’ve seen this firsthand. My grandma was on oxycodone for ‘arthritis’-turned out she was just dizzy all day, barely ate, kept falling. We tapered her off slowly, started her on heat packs and physical therapy. She started laughing again. Didn’t need the pills. Doctors don’t always listen, but families can push back. You don’t have to accept ‘it’s just aging.’
Ajay Sangani December 27 2025
isnt it strange how we treat pain like its a problem to be solved with chemicals when maybe its a signal? the body is trying to tell us something-move less, rest more, change your life. we just throw pills at it and call it medicine. and then wonder why old people are confused and falling. maybe the real epidemic isnt opioids… its our refusal to sit with discomfort.
Pankaj Chaudhary IPS December 28 2025
In India, we see this too-elderly patients on long-term opioids prescribed without proper evaluation. Family members often pressure doctors to ‘do something’ for pain, and doctors, fearing complaints, comply. But we must educate: non-pharmacological interventions like yoga, Ayurvedic massage, and community-based physiotherapy are not alternatives-they are the foundation. We need geriatric pain clinics in every district hospital. This is not just medical-it is cultural.
Gray Dedoiko December 30 2025
My dad was on tramadol for 3 years after knee surgery. He didn’t even realize he was getting more confused until his grandkid asked why he kept forgetting her name. We cut it out over 6 weeks. He’s been better since. Honestly? I didn’t know any of this stuff until it happened to us. Thanks for posting this-it’s the kind of info that saves lives.
Bartholomew Henry Allen December 30 2025
Stop coddling the elderly with feel good nonsense. Pain is weakness leaving the body. If they can't handle a little drowsiness then they should have exercised more when they were young. Opioids are not the enemy. Weakness is. America is turning into a nation of fragile people who need hand holding instead of grit
bharath vinay December 31 2025
Did you know that the CDC guidelines were written by pharmaceutical consultants? The whole opioid scare is a distraction. The real issue is that nursing homes are understaffed so they give opioids to keep seniors quiet. The falls? That’s from nurses not helping them walk. The delirium? That’s from anticholinergics in their sleep meds. Opioids are being blamed for systemic failures. And the media loves a villain.
Usha Sundar January 1 2026
My aunt took opioids for 8 years. One day she just… stopped talking. They said it was dementia. It wasn’t. It was the drugs. She died 6 months later.
Abby Polhill January 3 2026
Interesting how the data mirrors what we see in geriatric clinics-especially the CYP2D6 interactions with SSRIs. Tramadol + sertraline = walking time bomb. And yet, so many prescribers still don’t check drug interaction databases. We need mandatory EHR alerts. Also-topical capsaicin is underused. So simple. So effective. Why isn’t this in every primary care formulary?
Lindsey Kidd January 3 2026
💖 I’m so glad this is getting attention. My mom’s pain management team finally switched her to gabapentin + daily walks + acupuncture. She’s smiling again. No more confusion. No more falls. Just… her. Thank you for writing this. 💖
Bret Freeman January 4 2026
This is the most important public health issue no one’s talking about. I’ve seen grandparents become ghosts in their own homes because of a script. And the worst part? They’re too scared to speak up. ‘I don’t want to be a burden.’ We need to change that. We need to teach families to ask: ‘Is this helping or hurting?’ And we need to make deprescribing a normal, celebrated part of care-not a failure. This isn’t just medicine. It’s love.