When you take an SSRI antidepressant like sertraline or escitalopram, it’s meant to help you feel better. But what if something you take on top of it-maybe a painkiller, a cold medicine, or even a herbal supplement-pushes your serotonin levels too high? That’s when serotonin syndrome can happen. It’s not rare. It’s not theoretical. And it can kill you.
What Exactly Is Serotonin Syndrome?
Serotonin syndrome isn’t just feeling a little jittery. It’s a medical emergency caused by too much serotonin building up in your brain and nervous system. Think of serotonin as a chemical messenger. SSRIs stop your brain from reabsorbing it, so more stays active. That’s how they help with depression. But when other drugs add even more serotonin-or block its breakdown-the system overloads. Symptoms show up fast. Sometimes within hours. You might start shivering, sweating like you’re running a fever, your muscles turn stiff, your heart races, or you get confused. In severe cases, your body temperature spikes above 104°F, seizures happen, and your organs begin to shut down. The Hunter Serotonin Toxicity Criteria are what doctors use to diagnose it: if you have clonus (involuntary muscle spasms) plus fever or agitation, or rigid muscles with a high temperature and clonus-you’re likely in serotonin syndrome. It’s underdiagnosed because many symptoms look like the flu, a panic attack, or even drug withdrawal. But when it’s real, every minute counts.Which Medications Are the Biggest Risks?
Not all drug combinations are equal. Some are dangerous. Others are fine. Here’s what the data says. MAOIs are the deadliest. Mixing an SSRI with an MAOI like phenelzine or selegiline is a hard no. This combination has caused dozens of deaths. The risk is so high that doctors require a 2-week gap (or 5 weeks if you’re coming off fluoxetine) before switching between them. The FDA and European Medicines Agency both list this as a contraindication. Tramadol, dextromethorphan, and pethidine are high-risk opioids. Tramadol is especially sneaky. It’s often prescribed for mild to moderate pain, and many people think it’s safe because it’s not oxycodone or hydrocodone. But tramadol boosts serotonin and blocks its reuptake-just like an SSRI. A 2023 study found people taking tramadol with an SSRI had nearly 5 times the risk of serotonin syndrome. One Reddit user described being hospitalized after taking tramadol with sertraline: muscle rigidity, 104.2°F fever, and uncontrollable leg movements. That’s not an exaggeration. That’s a documented case. Linezolid, an antibiotic, is a hidden danger. If you’re on an SSRI and get a stubborn infection, your doctor might prescribe linezolid. It’s an MAOI-like drug. A 2022 JAMA study found that in older adults, combining linezolid with antidepressants led to serotonin syndrome in 0.14% of cases-low, but real. And when it happens, it’s often severe. SNRIs like venlafaxine or duloxetine can be risky too. They work like SSRIs but also affect norepinephrine. Combining them with SSRIs doesn’t just double the dose-it multiplies the risk. A 2023 study showed this combo increased serotonin syndrome risk by 3.2 times. St. John’s wort, tryptophan, and 5-HTP? Avoid them. These herbal supplements are sold as “natural mood boosters.” But they directly raise serotonin. One user on Drugs.com said they got shaking and confusion after taking St. John’s wort with Prozac-just three days in. The ER diagnosed early serotonin syndrome. No warning label on the bottle told them that.What About Other Opioids?
Not all pain meds are equal. Morphine, codeine, oxycodone, and buprenorphine don’t significantly raise serotonin levels. Studies show their risk is near zero when taken with SSRIs. That’s why the CDC’s 2024 opioid prescribing guidelines now recommend these over tramadol or dextromethorphan for patients on antidepressants. Methadone and fentanyl? Medium risk. They can contribute, especially at high doses or in older adults. But they’re not automatic red flags like tramadol.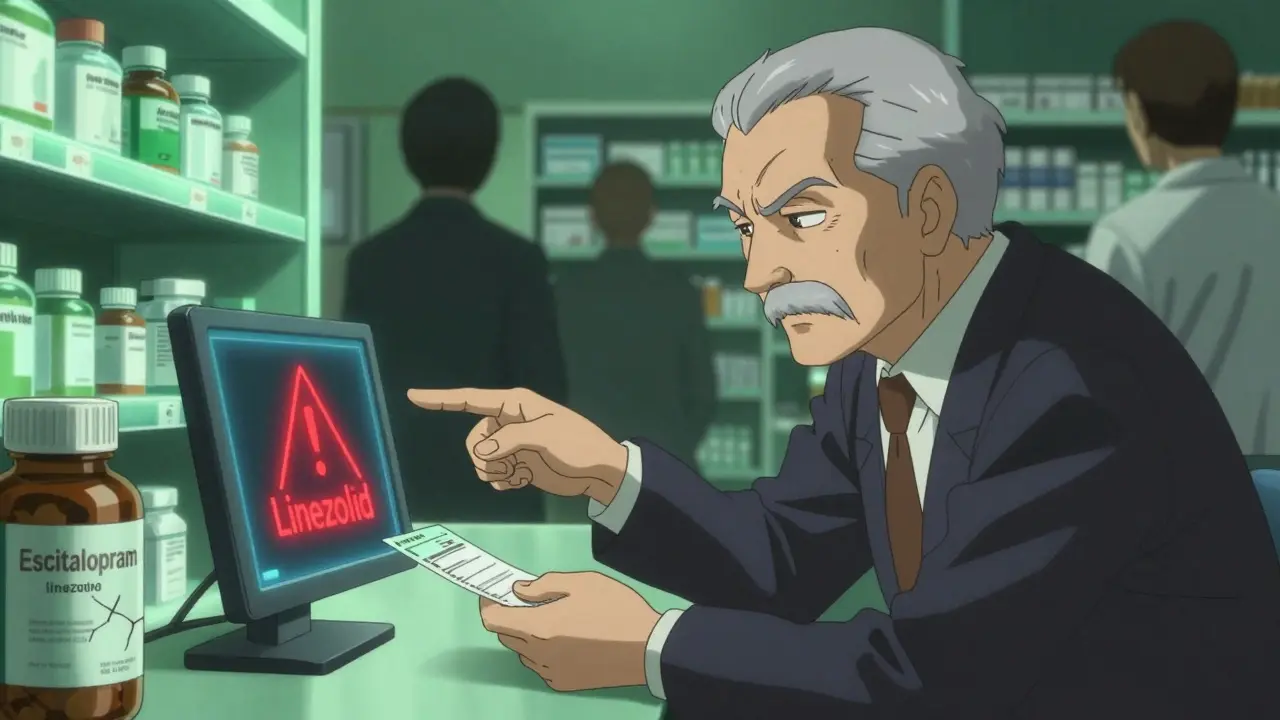
Who’s Most at Risk?
It’s not just about what you take-it’s who you are. People over 65 are at higher risk. Why? Because they’re more likely to be on multiple medications. One in five Americans over 60 takes an SSRI. One in five also takes an opioid. And nearly a quarter take five or more drugs daily. That’s a perfect storm. Genetics matter too. Some people are CYP2D6 poor metabolizers. Their bodies can’t break down tramadol or other drugs properly. That means more serotonin hangs around longer. A 2023 UCSF study found these people had 2.4 times the risk of serotonin syndrome when taking tramadol with an SSRI. And then there’s the system. A 2023 study found that 68% of serotonin syndrome cases reported to the FDA involved multiple medications. Many were prescribing errors. One patient got tramadol from their primary care doctor and sertraline from their psychiatrist. Neither knew the other had prescribed something.How to Stay Safe
You don’t have to live in fear. But you do need to be smart.- Know your meds. If you’re on an SSRI, make a list of everything you take-even OTC stuff and supplements. Bring it to every appointment.
- Ask your pharmacist. Pharmacists are trained to catch dangerous combinations. A 2023 study showed pharmacist-led reviews cut serotonin syndrome events by 47% in Medicare patients.
- Watch for the 5 S’s. Shivering, Sweating, Stiffness, Seizures (rare), and Sudden confusion. If you notice these after starting a new drug, stop it and call your doctor immediately.
- Never mix SSRIs with MAOIs. Not even for a day. Not even if you’re “just trying something new.”
- Ask before taking new painkillers. If your doctor prescribes a new opioid, ask: “Is this safe with my SSRI?” If they say yes, ask which one they recommend. Oxycodone or morphine are safer than tramadol.
What’s Changing?
The system is catching up. In 2024, the FDA mandated that all electronic prescribing systems must show real-time alerts when a doctor tries to prescribe an SSRI with tramadol, linezolid, or an MAOI. Epic Systems already did this in 2022-and cut risky prescriptions by 32% across 200 hospitals. A new blood test called SerotoninQuant is in phase 3 trials. By 2026, it might give doctors an objective way to confirm serotonin syndrome instead of guessing based on symptoms. But until then, the safest thing you can do is stay informed.What If You Think You Have It?
If you’re experiencing symptoms-especially muscle rigidity, high fever, or confusion-go to the ER. Don’t wait. Don’t call your doctor tomorrow. Go now. Treatment is simple but urgent: stop the offending drugs, give IV fluids, and use benzodiazepines to calm the nervous system. In severe cases, doctors may use cyproheptadine, an antihistamine that blocks serotonin. The key is speed. Hospital stays average $28,745 per case. But the real cost? If you wait too long, it’s your life.Bottom Line
SSRIs are life-changing for millions. But they’re not harmless. Their biggest danger isn’t side effects-it’s what they do when mixed with other drugs. Tramadol, St. John’s wort, MAOIs, linezolid-these aren’t just “possible” risks. They’re proven killers. You don’t need to avoid SSRIs. But you do need to treat them like any other powerful medicine. Ask questions. Know your list. Speak up. Your life might depend on it.Can you get serotonin syndrome from just one SSRI?
It’s extremely rare. Serotonin syndrome almost always happens when SSRIs are combined with another serotonergic drug. There are isolated reports of overdose causing it-like taking 10 times the normal dose of fluoxetine-but these are medical emergencies, not typical side effects. For most people, the risk only becomes real when two or more serotonin-boosting substances are taken together.
How long does it take for serotonin syndrome to go away?
Mild cases often resolve within 24 to 72 hours after stopping the offending drug. Symptoms like shivering and sweating fade first. Muscle stiffness and confusion take longer. Severe cases may require ICU care and can last days to weeks, especially if the drug has a long half-life like fluoxetine. Recovery depends on how quickly treatment starts and how much serotonin built up.
Is it safe to take melatonin with an SSRI?
Yes. Melatonin doesn’t affect serotonin levels in the way that triggers serotonin syndrome. It’s a hormone that regulates sleep, not a serotonin reuptake inhibitor. Multiple studies and clinical guidelines confirm it’s safe to use with SSRIs. Many people take it to help with sleep side effects from antidepressants.
Do all SSRIs carry the same risk?
No. Paroxetine has the strongest serotonin reuptake inhibition, making it slightly more likely to cause issues in combination. Fluoxetine lasts the longest in your body-up to two weeks after you stop taking it-so the interaction window is wider. Sertraline and escitalopram are generally considered lower risk, but no SSRI is risk-free when mixed with other serotonergic drugs.
Can serotonin syndrome happen after stopping an SSRI?
Yes, but only if you start another serotonergic drug too soon after stopping. For example, if you quit fluoxetine and then take tramadol a week later, you’re still at risk because fluoxetine sticks around for weeks. The standard advice is to wait 5 weeks after fluoxetine before starting an MAOI or other high-risk drug. For other SSRIs, 2 weeks is usually enough.
Should I stop my SSRI if I need surgery?
Usually not. Many anesthetics and pain meds used during surgery are safe with SSRIs. But you must tell your anesthesiologist you’re on an SSRI. They’ll avoid drugs like meperidine (pethidine) and tramadol. If you’re on fluoxetine, they may delay surgery to allow for a longer washout. Never stop your SSRI without consulting your prescriber-sudden withdrawal can cause its own dangerous symptoms.