More than 1 in 10 people in the U.S. think they’re allergic to a drug. But here’s the catch: most of them aren’t. A rash after taking amoxicillin? Maybe. A swollen throat after penicillin? That’s serious. The difference between a side effect and a true drug allergy can mean the difference between getting the right treatment-or being stuck with something less effective, more expensive, and riskier.
What Exactly Is a Drug Allergy?
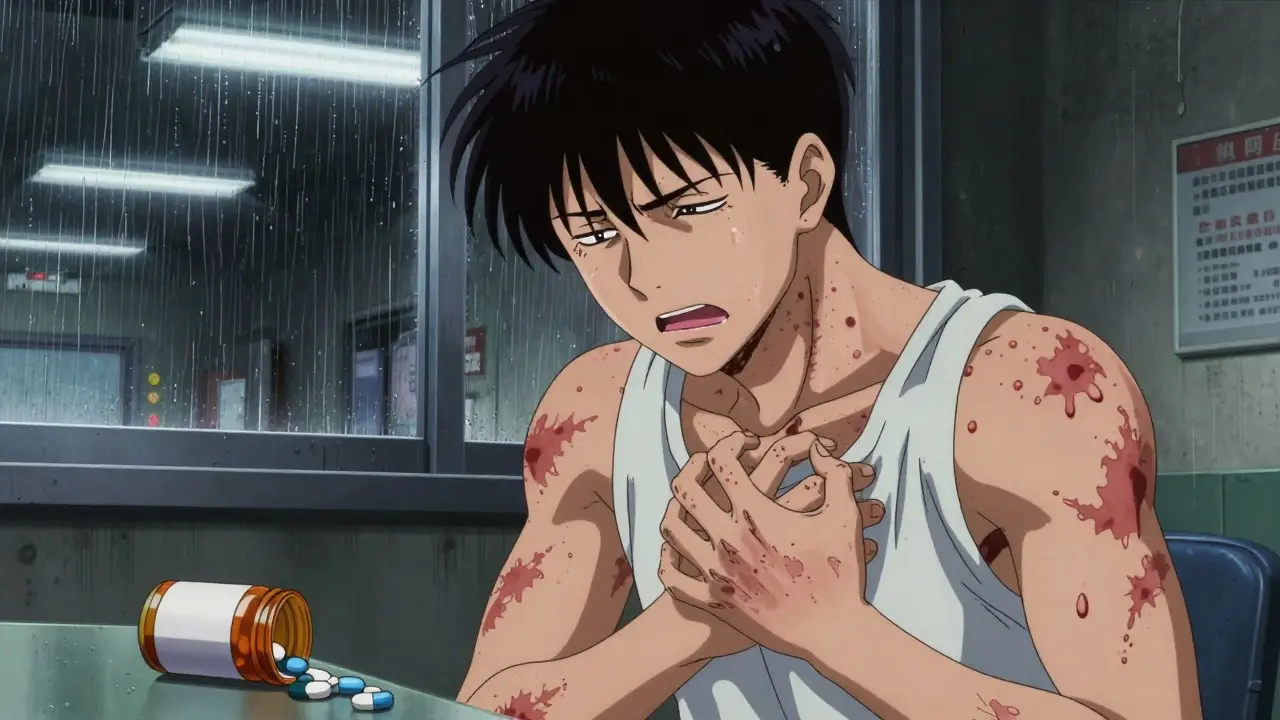
A drug allergy isn’t just a bad reaction. It’s your immune system mistaking a medication for a threat and launching a full attack. That’s different from side effects like nausea or dizziness, which happen because of how the drug works in your body-not because your immune system is involved. True drug allergies are rare. But when they happen, they can be life-threatening. The most common sign? A skin reaction. Rashes, hives, itching-these show up in nearly every case. But not all rashes are allergies. Some come from viruses, heat, or even just irritation. The key is timing and other symptoms.Common Signs of a Drug Allergy
Symptoms vary widely, but here’s what to watch for:- Hives: Raised, red, itchy welts that can appear anywhere on the skin. They may come and go quickly.
- Itching: Not just mild. Think intense, widespread, and unrelenting-even without a visible rash.
- Swelling: Lips, tongue, eyelids, throat. Swelling in the throat is a red flag.
- Difficulty breathing: Wheezing, tight chest, feeling like you can’t get air. This isn’t just a cold.
- GI symptoms: Vomiting, diarrhea, cramps. These can happen alone or with skin issues.
- Fever: Especially if it shows up days or weeks after starting a drug.
- Blistering or peeling skin: This is serious. If your skin starts coming off in sheets, get help now.
Timing Matters: When Do Symptoms Show Up?
Drug reactions don’t all happen the same way. The timing tells you what you’re dealing with:- Immediate (within minutes to 1 hour): This is IgE-mediated-anaphylaxis territory. Hives, swelling, trouble breathing, low blood pressure. This is an emergency.
- Delayed (1-6 hours): Still serious. Could be a mix of hives, vomiting, wheezing. Often mistaken for a virus.
- Days later (3-14 days): This is often a drug exanthem-a flat or bumpy rash. Common with antibiotics like penicillin or sulfa drugs. Usually not life-threatening but still needs evaluation.
- Weeks later (1-3 weeks): Could be serum sickness or DRESS syndrome. Fever, swollen lymph nodes, joint pain, liver problems. DRESS can damage organs and needs hospital care.
When to Call 911 or Go to the ER
If you’re taking a drug and suddenly feel like your body is shutting down, don’t wait. Call 911 if you have:- Swelling of the tongue or throat
- Difficulty breathing or wheezing
- Dizziness, fainting, or feeling like you’re going to pass out
- A combination of symptoms-like a rash + vomiting + trouble breathing

What About That Rash After Amoxicillin?
Penicillin and related antibiotics are the most commonly reported drug allergies. But here’s the surprise: over 90% of people who say they’re allergic to penicillin aren’t. Many got a rash as a kid, were told they were allergic, and never got tested. A true penicillin allergy means a reaction that involved hives, swelling, or breathing trouble-not just a mild rash. If you’ve been avoiding penicillin for years because of a childhood rash, you might be missing out on the safest, cheapest, most effective antibiotic for your infection. Skin testing for penicillin is reliable. If the test is negative, you might get a small oral dose under supervision to confirm. Most people pass. That means you can go back to using penicillin-avoiding stronger, costlier, and riskier antibiotics.How Doctors Diagnose Drug Allergies
There’s no blood test for most drug allergies. That’s why diagnosis is so tricky.- History is everything: Your doctor will ask: When did the reaction happen? What did it look like? Did you have fever or swelling? Did you take any other meds? Did it get better after stopping the drug?
- Physical exam: They’ll look at your skin, check your airways, listen to your lungs.
- Photographs: If you can’t get to the doctor right away, take clear pictures of the rash. It might be gone by the time you see someone.
- Penicillin skin testing: This is the only widely accepted test. Done in an allergist’s office. They prick your skin with tiny amounts of penicillin. If you’re allergic, you’ll get a raised bump.
- Oral challenge: If skin tests are negative, you might be given a small dose of the drug under watch. This is the gold standard for ruling out an allergy.
- Blood tests: Only useful for rare, delayed reactions like DRESS. They check for high eosinophils or liver enzymes.
Why Mislabeling Is Dangerous
Being wrongly labeled as allergic to penicillin doesn’t just mean you avoid one drug. It means you get something else-often a broader-spectrum antibiotic like vancomycin or ciprofloxacin. These drugs:- Cost more
- Have more side effects
- Lead to more hospital stays
- Increase your risk of C. diff infection-a severe, sometimes deadly gut infection

What to Do After a Reaction
If you had a mild reaction-just a rash with no breathing trouble-don’t panic. But don’t ignore it either.- Stop the drug.
- Take a picture of the rash.
- Call your doctor. Don’t wait for it to get worse.
- Ask: Could this be an allergy? Should I see an allergist?
What to Tell Your Doctor
When you describe a reaction, be specific:- What drug? (Name and dose)
- When did you take it?
- How long until symptoms started?
- What exactly happened? (Rash? Swelling? Trouble breathing? Vomiting?)
- Did you take any other meds or supplements?
- Did it go away after stopping the drug?
- Did you have fever, swollen glands, or joint pain?
What You Should Never Do
- Don’t assume you’re allergic just because someone else had a reaction.
- Don’t avoid a drug because your grandma said she was allergic to it.
- Don’t ignore a rash because you think it’s "just a reaction."
- Don’t take the same drug again after a serious reaction without seeing an allergist.
- Don’t skip follow-up testing. Many people live with unnecessary restrictions for decades.
Final Thought: Don’t Guess. Get Tested.
If you’ve ever had a reaction to a drug, especially one that involved swelling, breathing trouble, or blistering skin-get it checked. You might be carrying around a label that’s holding you back from the best care possible. And if you’ve been told you’re allergic to penicillin? Ask about testing. It’s safe. It’s simple. And it could change your medical future.How do I know if my rash is a drug allergy or just a side effect?
A side effect usually doesn’t involve your immune system. Think nausea, dizziness, or mild headache. A drug allergy means your body is mounting an immune response. Look for hives, swelling, trouble breathing, or blistering skin. If you have more than one symptom-like a rash plus vomiting or wheezing-it’s more likely an allergy. Timing matters too: side effects often happen right away; allergies can take hours or days.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Studies show that up to 80% of people who were allergic to penicillin as kids lose the allergy after 10 years. But you shouldn’t assume you’re no longer allergic. The only way to know for sure is through proper testing by an allergist. Don’t just try the drug again on your own.
Is there a blood test for drug allergies?
For most drugs, no. Blood tests aren’t reliable for diagnosing allergies to common medications like penicillin or ibuprofen. The exception is for rare, delayed reactions like DRESS syndrome, where doctors might check for high levels of eosinophils or liver enzymes. For most cases, diagnosis is based on your history and physical exam. Skin testing is the gold standard-for penicillin only.
What should I do if I think I’m having an allergic reaction?
If symptoms are mild-like a rash or itching-stop the drug and call your doctor. Take a photo of the rash. If you have trouble breathing, swelling in your throat, dizziness, or feel like you’re going to pass out-call 911 immediately. Use an EpiPen if you have one. Don’t wait to see if it gets better. Anaphylaxis can kill in minutes.
Can I take other drugs if I’m allergic to one?
Maybe. Drug allergies are usually specific to one drug or a very similar group. Being allergic to penicillin doesn’t mean you’re allergic to all antibiotics. But some drugs in the same class (like amoxicillin or cephalexin) might trigger a reaction. Always tell your doctor exactly what you reacted to. They’ll check cross-reactivity risks before prescribing anything new.
Should I wear a medical alert bracelet for a drug allergy?
Yes-if you’ve had a serious reaction like anaphylaxis, swelling, or blistering skin. A medical alert bracelet can save your life if you’re ever unconscious in an emergency. Write the exact drug and reaction: "Penicillin: Anaphylaxis" or "Sulfa: Stevens-Johnson Syndrome." Avoid vague terms like "drug allergy." Be specific.
Can I be tested for allergies to all drugs?
No. Only penicillin and a few others have reliable tests. For most drugs, there’s no standard test. Diagnosis is based on your history and symptoms. If you’ve had a serious reaction, an allergist can help determine what’s safe based on your pattern of reactions. They may do an oral challenge under supervision if it’s low-risk.
What’s the difference between a drug allergy and a drug intolerance?
A drug allergy involves your immune system. It can cause hives, swelling, or anaphylaxis. A drug intolerance is when your body doesn’t handle the drug well, but your immune system isn’t involved. Think stomach upset from ibuprofen or dizziness from blood pressure meds. Intolerances are common. Allergies are rare-but far more dangerous.
15 Comments
Pankaj Singh January 14 2026
This is just basic medical propaganda. 90% of people aren't allergic to penicillin? So what? You're telling me we should just trust some skin test instead of decades of lived experience? I've seen people swell up like balloons. Don't play with fire.
Scottie Baker January 15 2026
I took amoxicillin in 2012 and broke out in hives. They told me I was allergic. Fast forward 10 years, I get tested and turns out I'm fine. Now I'm on penicillin for my sinus infection and it's working like a charm. Why didn't anyone tell me this sooner?
Diana Campos Ortiz January 16 2026
i got a rash after amoxicillin when i was 7. my mom said i'm allergic. i never questioned it. until last year when i had to get surgery and they said "wait, you're not allergic" and i just... cried. like, why did i avoid the best antibiotic for 20 years? this post saved me.
Jesse Ibarra January 17 2026
You people are so naive. Allergists make bank off these "tests." They don't care if you're mislabeled-they care if you come back for the next appointment. This isn't science, it's a $$$ pipeline.
laura Drever January 19 2026
penicillin allergy is a myth. also i think the author is just trying to sell more tests. i dont trust doctors anymore.
jefferson fernandes January 21 2026
If you've ever had a reaction, please-don't just assume. Talk to an allergist. Seriously. I had a cousin who avoided all antibiotics for 15 years because of a childhood rash. Got C. diff three times. She finally got tested last year. Turns out she's fine. Now she's alive. That's not luck. That's science.
Nelly Oruko January 22 2026
It's fascinating how we've built entire medical protocols around assumptions. We label people with allergies based on a single rash, then treat them as if they're radioactive to entire drug classes. And yet, the immune system is so precise-it doesn't just "hate" a molecule because it looks similar. We need to stop treating biology like a spreadsheet. Testing isn't optional. It's ethical.
Vinaypriy Wane January 23 2026
I'm a nurse. I've seen this too many times. A patient comes in with a penicillin allergy label, gets vancomycin, gets diarrhea, ends up in ICU. We spend 10x more money. We risk their life. And it all started because someone's kid got a rash at age 4. Please. Get tested. It's 15 minutes. It's safe. It's free in most places. Don't be the reason your kid gets a C. diff infection because you didn't ask.
Trevor Davis January 24 2026
My grandma had a rash after penicillin in 1962. She told my mom. My mom told me. I avoided it for 30 years. Last year, I got tested. Negative. I took a dose under supervision. Felt fine. Now I'm on amoxicillin for a UTI. I feel like I just got my medical freedom back. Thank you for this. I wish I'd known sooner.
Acacia Hendrix January 24 2026
The diagnostic paradigm is fundamentally flawed. The IgE-mediated response is only one axis of immune dysregulation. The delayed hypersensitivity reactions-like DRESS and SJS-are often misclassified as "side effects" because clinicians lack the immunological literacy to parse them. We need standardized biomarker panels, not anecdotal history-taking. This post is a start, but it's still stuck in the 20th century.
Lance Nickie January 25 2026
so penicillin allergy is fake? then why do i get dizzy when i take it? maybe its just me being sensitive? or maybe its the placebo effect? idk. but i still wont take it.
Milla Masliy January 25 2026
In my village in Nigeria, we say: "If it makes you itch, it’s not for you." But here in the States, people get tested for allergies like they’re choosing a Netflix plan. We need both wisdom and science. Don’t ignore your body-but don’t let fear write your prescription either.
Angel Molano January 26 2026
You’re telling people to trust doctors after what happened with Vioxx? With OxyContin? With the flu vaccine lies? You’re not educating. You’re brainwashing.
Lethabo Phalafala January 26 2026
I had a reaction to cipro that turned into Stevens-Johnson. My skin peeled off. I was in the hospital for 3 weeks. I will NEVER take another fluoroquinolone. Ever. And if you tell me to get tested for it? No. That’s not an allergy. That’s a near-death experience. Some labels aren’t mistakes. They’re survival.
Damario Brown January 27 2026
I work in ER. Last week, a guy came in with hives and swelling. Said he was allergic to penicillin. We gave him cefdinir anyway. He coded. Turned out he was never allergic. The real allergy? The doctor who didn't check his chart. This isn't about tests. It's about lazy medicine. And people are dying because of it.