When you pick up a prescription for a combination drug like metformin/sitagliptin or fluticasone/salmeterol, you might assume the generic version is just as good as the brand name. After all, the active ingredients are the same. But what if the problem isn’t what’s in the pill-or the inhaler-but what’s not in it? The truth is, generic combinations can differ significantly from brand versions in their inactive ingredients, and for some patients, that difference matters more than you’d think.
Why Generic Combinations Aren’t Always Identical
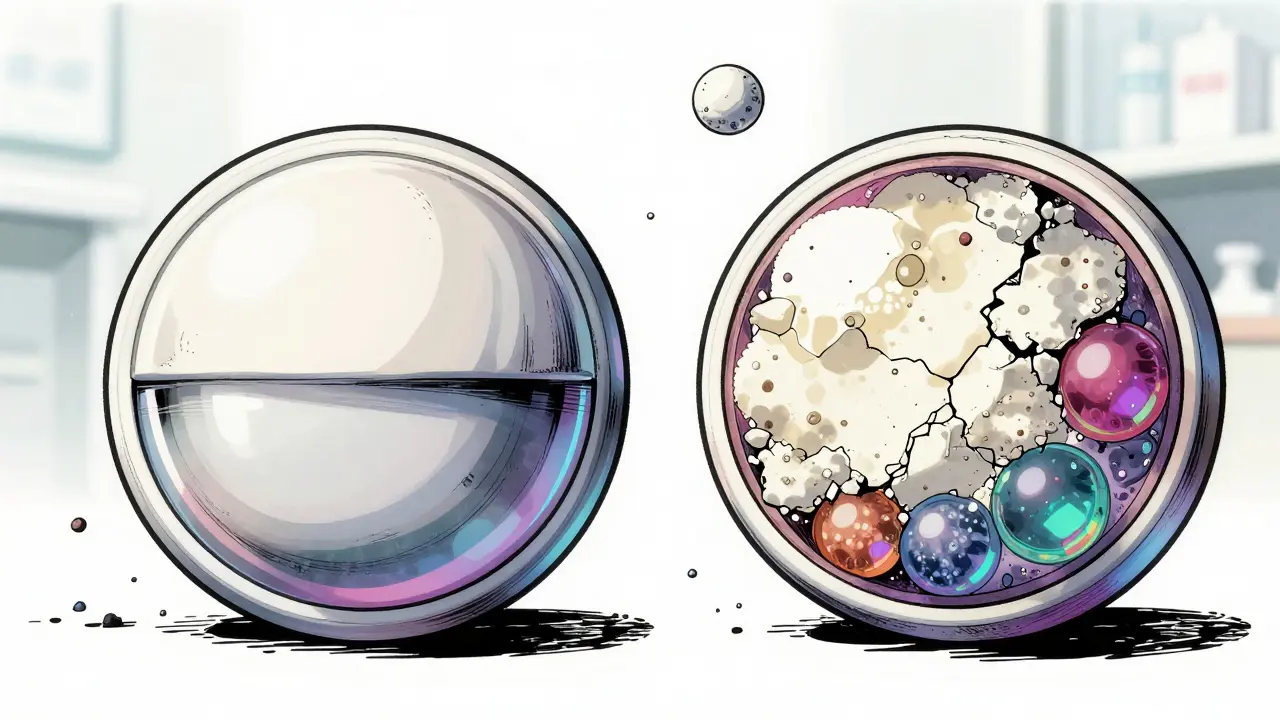
The FDA requires generic drugs to have the same active ingredients, strength, dosage form, and route of administration as the brand-name version. That’s the law. But it doesn’t require them to have the same fillers, binders, dyes, or coatings. These are called inactive ingredients, and they play a bigger role than most people realize. Take magnesium stearate, a common lubricant used in tablets. It’s harmless for most people. But in one 2017 study, 38% of generic combination drugs had a different type or amount of this ingredient than the brand version. For someone with a sensitive gut, that small change could mean more bloating, nausea, or diarrhea. Lactose is another example. About 29% of generics use different levels of lactose than the brand. For patients with lactose intolerance, even a tiny amount can trigger symptoms-something the brand version might have avoided entirely. And it’s not just pills. Inhalers like Advair Diskus contain complex delivery systems. A 2021 study found that some generic versions delivered 15-20% less medication to the lungs because the device’s internal mechanics differed slightly. The active ingredients were the same, but the way they reached the lungs wasn’t. That’s why some patients reported needing their rescue inhaler more often after switching.When the Difference Actually Matters
Not all drugs are created equal when it comes to substitution risk. The FDA classifies certain medications as having a narrow therapeutic index (NTI). These are drugs where even a small change in blood levels can lead to treatment failure or serious side effects. Examples include warfarin, levothyroxine, and some anti-seizure medications. For combination NTI drugs, the risks multiply. A 2020 study of nearly 90,000 Medicare patients switching from brand to generic levothyroxine found that 12.3% needed a dosage adjustment because their thyroid hormone levels changed. That’s more than one in eight patients. And while most people tolerate the switch fine, for those who don’t, the consequences can be fatigue, heart palpitations, or even hospitalization. Combination drugs like lamotrigine/levetiracetam for epilepsy or olmesartan/hydrochlorothiazide for high blood pressure fall into this high-risk category. The FDA lists only 14 NTI drugs, but combination versions of these are growing. And because they’re often taken long-term, small changes in absorption can build up over time.What the Data Shows: Real Patient Experiences
Behind the statistics are real people. On PatientsLikeMe, over 23% of users who switched to generic combination drugs reported new or worsening side effects. The highest complaint rates came from those on psychiatric meds (31.2%) and thyroid treatments (28.6%). Reddit’s r/pharmacy community collected 478 case reports in 2022. Over 60% involved combination drugs. One user described switching from Janumet (metformin/sitagliptin) to the generic and suddenly developing severe stomach cramps and diarrhea-something they’d never experienced on the brand. Another reported panic attacks after switching from a generic version of a combination antidepressant. Their doctor couldn’t explain it-until they switched back. Pharmacists are hearing this too. A 2022 survey found that 34% of independent pharmacists received patient complaints about generic combinations. The top issues? Gastrointestinal upset (41%), skin rashes (29%), and feeling like the medication “just doesn’t work anymore” (22%).
How to Know If You’re at Risk
The first step is understanding your medication. Check the Orange Book-the FDA’s official list of approved generics and their therapeutic equivalence ratings. If your drug has an “A” rating, it’s generally considered interchangeable. If it has a “B” rating, proceed with caution. Ask your pharmacist: “Is this generic the same as the brand in every way?” They can check the inactive ingredients. Some pharmacies now print these on the label. If not, request a copy of the manufacturer’s product insert. Look for differences in:- Lactose, gluten, or dyes
- Extended-release coatings
- Tablet shape or size (can affect swallowing or dissolution)
- Inhaler device mechanics (for combination inhalers)
What You Can Do: A Five-Point Safety Checklist
Pharmacists are now trained to use a simple five-point assessment before substituting a generic combination:- Therapeutic index - Is this a narrow index drug? (Check FDA list)
- Patient history - Have you ever had issues with a generic before?
- Active ingredient stability - Does your condition require tight control? (e.g., epilepsy, thyroid disease)
- Allergies - Are you allergic to any inactive ingredients? (Ask for the full list)
- Disease stability - Are you currently stable on the brand? Don’t rock the boat unless necessary.
12 Comments
Art Van Gelder December 23 2025
Man, I never thought about how the filler in my pills could be wrecking my gut. I switched to generic metformin/sitagliptin last year and started having these weird bloating spells-thought it was just my diet. Turns out, the generic had extra lactose and magnesium stearate. My pharmacist didn’t even mention it. Now I ask for the insert like it’s a damn rights thing. Feels like Big Pharma’s playing Jenga with our bodies and we’re the ones holding the blocks.
And don’t get me started on inhalers. I’ve got asthma. The brand one? Smooth. The generic? Like trying to breathe through a straw wrapped in duct tape. I swear, the device’s internal mechanics are different. No wonder people end up in the ER. We’re not just taking chemicals-we’re interacting with engineered systems. The FDA says ‘same active ingredients’ like that’s a magic wand. Nah. It’s a loophole with a stethoscope.
I’ve started keeping a symptom log. If I feel off after a refill? I go back to the brand. My insurance hates me. My body? Thankful. We need transparency. Not just ‘A’ ratings. We need ingredient-level transparency. Like nutrition labels on meds. I’d pay extra for that. My life isn’t a cost-cutting spreadsheet.
Also-why is no one talking about how the color dyes in generics trigger migraines? I’m not crazy. I’ve seen it. Purple tablets? Headache city. White ones? Fine. It’s not placebo. It’s physiology. We need research on this. Not just ‘it’s the same molecule.’ The molecule is just the headline. The rest is the damn novel.
Someone should start a subreddit: r/InactiveIngredientsMatter. I’ll mod it. I’ve got 478 case reports saved. I’m not just ranting. I’m archiving.
Nader Bsyouni December 24 2025
So you’re telling me the government lets companies swap out binders and call it the same drug and we’re supposed to trust this system because it’s legal
What a joke
It’s like saying two cars are identical because they both have four wheels and an engine
One’s a Tesla the other’s a 1998 Chevy Cavalier with duct tape on the door
And you wonder why people get sicker
Capitalism isn’t innovation it’s just rearranging the deck chairs on the Titanic while the FDA sips coffee and calls it ‘therapeutic equivalence’
Also I hate when people say ‘trust your doctor’
Your doctor works for a system that pays them to switch you to generics
They don’t care about your gut
They care about their bonus
Aliyu Sani December 25 2025
From Nigeria where we don’t even have reliable access to brand meds, this hits different. Here, even the generics are often substandard or counterfeit. But when we do get real generics, the variation in excipients? It’s a gamble. One guy I know with epilepsy had a seizure after switching to a ‘generic’ lamotrigine combo. Turned out the coating dissolved too fast-bioavailability went haywire. He almost died.
We need a global framework for inactive ingredient disclosure. Not just FDA. WHO should mandate this. Your body doesn’t care about borders. It reacts to starch, lactose, titanium dioxide the same whether you’re in Lagos or LA.
Also-why is no one studying how cultural diet affects drug absorption? A Nigerian with high cassava intake might metabolize meds differently than a Texan with a dairy-heavy diet. We’re treating pharmacology like it’s one-size-fits-all. It’s not. It’s biology + environment + corporate convenience.
And yes, I’ve seen patients cry because their ‘generic’ antidepressant made them feel ‘numb but not better.’ They don’t know why. The pharmacist shrugs. The system fails them. Again.
Gabriella da Silva Mendes December 27 2025
OMG I CANNOT BELIEVE THIS IS STILL A THING 😭😭😭
I switched to generic Advair and started wheezing like I was 12 again. My doctor said ‘it’s the same’ and I believed him. I was SO naive. I’m American. I paid taxes for this system. I deserve better. This is why I hate big pharma. They’re all greedy. They don’t care if you die as long as the stock price goes up 💸
Also I’m so proud of the U.S. for finally requiring inhaler testing in 2023. Finally someone’s doing something right. America still leads. 🇺🇸🇺🇸🇺🇸
PS I just posted a TikTok about this. 12k views in 2 hours. Someone needs to start a movement. #GenericMedicineIsAScam
Jim Brown December 28 2025
The philosophical underpinning of this issue lies not in pharmacology, but in epistemology: we are conditioned to equate equivalence with identity. A generic drug is not the same as its brand counterpart; it is a functional approximation, a shadow on the wall of the original form. The FDA’s regulatory framework, while legally sound, is epistemologically naive-it assumes biochemical sameness implies physiological sameness. But biology is not chemistry. Biology is context. Biology is the sum of a thousand silent variables: gut microbiota, epithelial permeability, genetic polymorphisms, even the time of day.
When a patient reports that the generic ‘doesn’t work anymore,’ they are not delusional. They are perceiving a difference the system refuses to acknowledge. The problem is not the patient’s sensitivity-it is the system’s arrogance.
We have quantified everything except the lived experience. We measure blood levels, not breathlessness. We track HbA1c, not fatigue. We approve formulations, not futures.
Perhaps the solution is not more regulation, but more humility. Let us admit that we do not fully understand how the body receives the drug. Let us honor the patient’s report as data. Let us make the inactive ingredients visible-not as an afterthought, but as the core of the therapeutic act.
Cara Hritz December 30 2025
Wait so you’re saying the generic version of my combo pill has different fillers? I thought generics were exact copies. My pharmacist said they were. She must’ve been lying. Or maybe I misheard. I’m kinda bad with names. Anyway, I’ve been on this med for 5 years and I’ve never had a problem until last month. Now I’m tired all the time and my skin is breaking out. Could it be the dye? I think I saw a red dot on the pill. Maybe it’s gluten? I think I’m allergic to gluten? Or maybe I’m just stressed. I don’t know. I’m gonna call my doctor. But I’m also mad at the pharmacy. They should’ve told me. This is so confusing. I just want to feel normal again.
Johnnie R. Bailey December 30 2025
I’ve been a pharmacist for 22 years. I’ve seen this play out a hundred times. The system is broken, not because generics are bad-but because we treat them like interchangeable widgets. We don’t have the tools to predict who will react. We don’t have the time to educate. We don’t have the reimbursement to document.
But here’s what I do: I keep a binder. Every time a patient tells me they felt different after a switch, I write it down-med name, manufacturer, inactive ingredients, symptoms, date. I’ve got 87 entries. Over half are combination drugs. Two patients had seizures. One nearly died from thyroid crash. None were flagged by the system.
I’ve started asking patients: ‘Have you ever had a bad reaction to a generic?’ If yes? I refuse to substitute. I don’t care if it’s cheaper. I don’t care if the insurance says ‘automatic substitution.’ I care that you’re alive.
And yes-I’ve had my share of pushback. But I’ve also had patients send me thank-you cards. One said, ‘You’re the only one who listened.’
Transparency isn’t a policy. It’s a promise. And we’re breaking it.
Kathryn Weymouth December 31 2025
Thank you for this thorough and necessary breakdown. The most alarming statistic for me was the 12.3% of Medicare patients requiring levothyroxine dosage adjustments after switching to generic. That’s not a fluke-it’s a systemic failure. The FDA’s ‘A’ rating system is misleading because it only assesses bioequivalence in healthy volunteers under controlled conditions. It doesn’t account for chronic illness, polypharmacy, or individual metabolic variance.
Additionally, the lack of mandatory labeling of inactive ingredients on prescription bottles is indefensible. If a food product must list every allergen, why shouldn’t a medication? The fact that patients must request a product insert to know what’s in their pill is a gross violation of informed consent.
As someone with Hashimoto’s, I switched to an authorized generic of levothyroxine after a similar experience. My TSH stabilized within six weeks. I wish I’d known about this option sooner. I urge every patient on NTI drugs to ask for the authorized generic-it’s the only way to guarantee identical formulation without paying brand price.
This isn’t anti-generic. It’s pro-patient. And it’s long overdue.
Julie Chavassieux January 1 2026
So... let me get this straight. You’re saying the pill I’ve been taking for 10 years might have changed without me knowing? And now I’m supposed to believe that the new one is ‘the same’? And the doctor just shrugs? And the pharmacist says ‘it’s FDA approved’? And we’re supposed to be grateful for the savings?
Let me tell you something. I have a 7-year-old with epilepsy. She’s been stable on her combo med since she was 2. Last month, the pharmacy switched her to generic. She had three seizures in 48 hours.
They said it was ‘coincidental.’
They said it was ‘stress.’
They said it was ‘probably not the meds.’
I pulled the bottle. The pill was a different color. Smaller. Smelled weird. I called the manufacturer. They said ‘minor formulation change.’
Minor.
My daughter almost died because of a ‘minor’ change.
I’m done trusting systems.
I’m done trusting doctors.
I’m done trusting ‘FDA approved.’
I’m buying the brand. Every month. And I’m telling every parent I know.
This isn’t about money.
This is about survival.
Herman Rousseau January 3 2026
Hey everyone-just wanted to say this is HUGE and I’m so glad someone finally put this out there. I’ve been telling my friends for years: don’t just accept a switch. Ask questions. Keep a journal. Track your sleep, your energy, your mood. I switched to generic for my BP med and felt like a zombie for 3 weeks. No one believed me until I showed them my log.
Now I always ask for the manufacturer’s name and check the Orange Book. I even screenshot the ingredient list and send it to my doctor. I’m not being ‘difficult.’ I’m being smart.
And if you’re on a combo med with a narrow therapeutic index? Don’t even think about switching unless you’re ready to fight for your life. You’re not being paranoid-you’re being prepared.
Also-authorized generics are a BLESSING. They’re like the brand but cheaper. Ask your pharmacist. They might not tell you unless you ask. I found mine for $18 instead of $80. Game changer.
You’ve got this. Stay informed. Stay loud. And never, ever let cost be the only decision.
❤️🩺
Vikrant Sura January 4 2026
So the data shows that 23% of patients report side effects after switching. That’s 1 in 4. But the sample size is self-selected from Reddit and PatientsLikeMe. That’s a biased population. People who have problems are more likely to report. Those who feel fine? They don’t post. So the real incidence is probably lower. Also, correlation ≠ causation. Maybe those patients were already declining. Also, the study didn’t control for adherence. Maybe they forgot to take it. Or drank grapefruit juice. Or started yoga. There’s too many confounders. This is anecdotal noise dressed as science.
Candy Cotton January 6 2026
As an American woman who has always supported innovation and American-made pharmaceuticals, I find it outrageous that foreign manufacturers are allowed to produce generics with inferior ingredients. We are sacrificing the health of our citizens for the sake of cost savings. This is not healthcare-it is corporate colonialism. The FDA should ban all foreign-made generics. Only American-made drugs should be allowed. We have the technology. We have the standards. Why are we letting other countries compromise our people’s lives? This is a national security issue. I urge Congress to act immediately.