When someone is having a severe allergic reaction, every second counts. Anaphylaxis can turn deadly in minutes - swelling in the throat, dropping blood pressure, trouble breathing. The only thing that can stop it in time is epinephrine. And the fastest way to give it? An epinephrine auto-injector. But if you’ve never used one before, it’s easy to freeze up. You’re scared. You’re in a panic. You don’t remember the steps. That’s why knowing exactly how to use it - not just in theory, but under pressure - could save a life.
What Happens During Anaphylaxis?
Anaphylaxis isn’t just a bad rash or a stuffy nose. It’s a full-body emergency. The immune system overreacts to something harmless - peanuts, bee stings, shellfish, even some medications - and floods the body with chemicals that cause blood vessels to leak, airways to tighten, and the heart to struggle. Symptoms can show up in seconds: hives, swelling of the lips or tongue, wheezing, dizziness, vomiting, or passing out. Without epinephrine, the body can shut down. Death can happen within 30 minutes.
That’s why guidelines from the American Academy of Allergy, Asthma & Immunology say epinephrine is the only first-line treatment. Antihistamines like Benadryl? They help with mild itching, but they won’t stop anaphylaxis. Waiting for them to work can cost someone their life. Studies show giving epinephrine within 5 to 15 minutes cuts the risk of dying by 75%.
Which Auto-Injectors Are Available?
You’ll most likely see one of four devices:
- EpiPen - The most common. Comes in 0.15mg (for kids 33-66 lbs) and 0.3mg (for anyone over 66 lbs). Has a bright orange tip that pops out when fired.
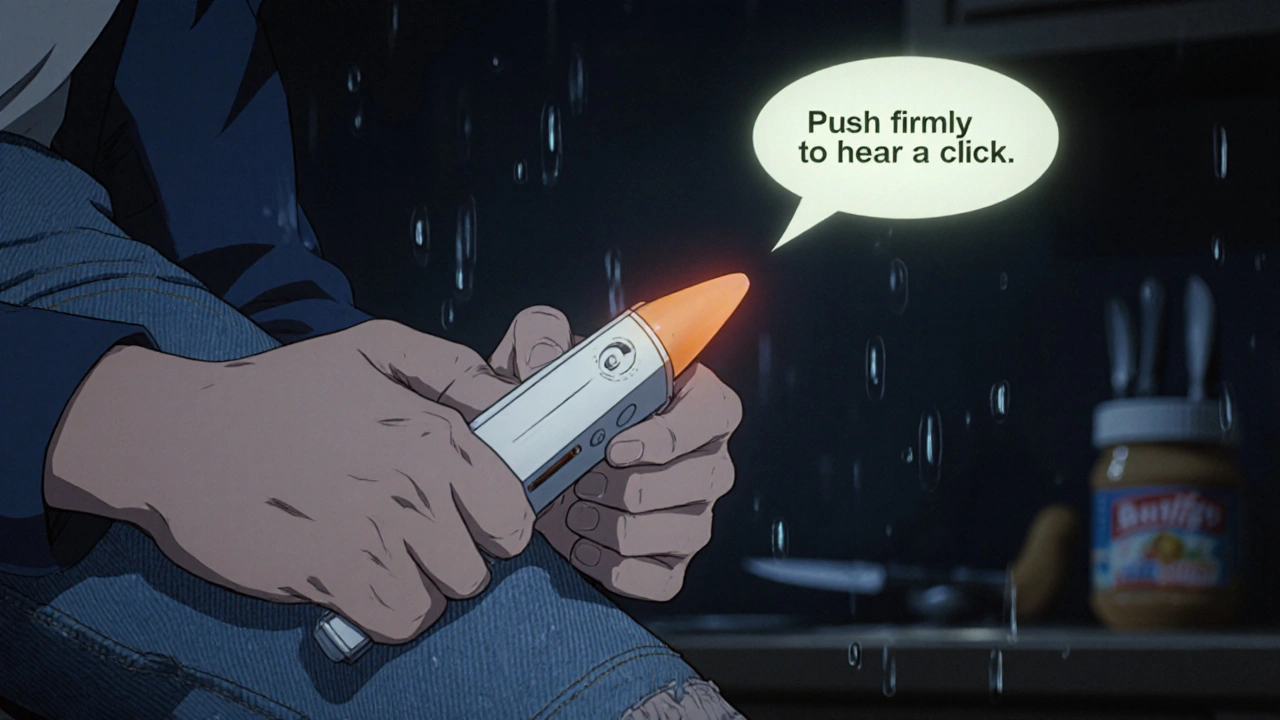
- Auvi-Q - Smaller, rectangular, and talks to you. Gives voice instructions like, “Pull off the red safety cap,” and “Push firmly until you hear a click.”
- Adrenaclick - Cheaper, but you have to remove two caps and manually push the plunger. Not as intuitive.
- Neffy - The newest. A nasal spray, no needle. Approved in 2023. Works for most people, but needs the right technique - you have to breathe in while spraying.
EpiPen still makes up over 85% of the market. But if you’re worried about needles, or if you’ve ever fumbled with the device, Auvi-Q’s voice prompts can make a huge difference. In one study, people using Auvi-Q got the dose right 89% of the time. With EpiPen, it was only 64%.
Step-by-Step: How to Use an Epinephrine Auto-Injector
There’s no room for guesswork. Here’s what to do - every time.
- Recognize the signs. Don’t wait for all symptoms. If someone has trouble breathing, swelling, or feels like they’re going to pass out - act now.
- Call 911. Even if you give the shot, they still need emergency care. Anaphylaxis can come back hours later.
- Remove the safety cap. For EpiPen and Auvi-Q, pull off the blue cap. For Adrenaclick, remove both the gray and black caps. Don’t cover the tip - you might accidentally trigger it.
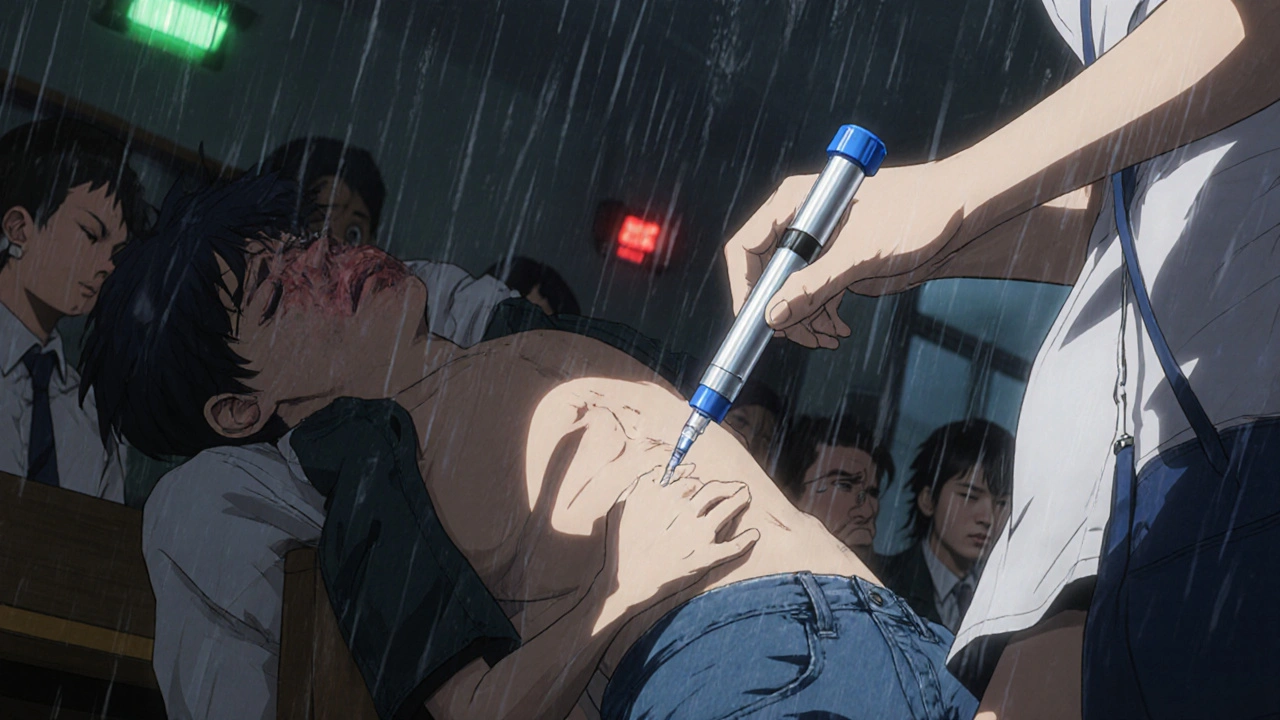
- Place it on the outer thigh. You can inject through clothing - jeans, leggings, even thick pants. No need to expose skin. The thigh is the best spot because it’s large, easy to reach, and has good blood flow.
- Push hard and hold. Jab it straight into the thigh. Don’t poke gently. You need to press until you hear or feel a click. Keep it pressed for 3 full seconds. That’s how long it takes to deliver the full dose. Don’t pull away early.
- Massage the area. After removing the injector, rub the injection site for 10 seconds. This helps the medicine get into the bloodstream faster.
- Call for help again if needed. If symptoms don’t improve after 5-10 minutes - or if they get worse - give a second dose. Most people only need one. But if the person is still struggling, a second shot is safe.
Important: Never inject into the hands, feet, buttocks, or veins. Never try to hold someone upright. Lay them flat. If they’re vomiting or having trouble breathing, turn them on their side. Standing up during a reaction can cause sudden blood pressure drops and lead to cardiac arrest.
Common Mistakes People Make
Even people who’ve been trained mess up. Here’s what goes wrong most often:
- Not holding it long enough. 61% of users pull the injector away before the 3 seconds are up. That means they get less than half the dose.
- Forgetting the safety cap. In school drills, 58% of nurses didn’t remove the blue cap before injecting.
- Injecting the wrong spot. Some people aim for the arm or stomach. The thigh is the only approved site.
- Waiting for other meds. Giving Benadryl first is a deadly delay. Epinephrine is the only thing that works.
- Not calling 911. People think once they give the shot, they’re fine. They’re not. Hospital care is still needed.
One study found that in real emergencies, only 42% of people got epinephrine on time. The rest waited - sometimes too long.
How to Practice - Without a Real Shot
Practice makes survival. You need to do this until it’s automatic.
Get a trainer device - they’re free from manufacturers. EpiPen, Auvi-Q, and Adrenaclick all send them out on request. These look like the real thing but don’t have a needle or medicine. Use them every few months.
Practice on an orange. Or a pillow. Or your own thigh. Do it while wearing clothes. Do it with one hand. Do it with your eyes closed. Train your family, your kids, your coworkers. Make it part of your routine - like checking your smoke alarm.
Simulation studies show you need about 3-4 practice sessions to get 90% accuracy. Don’t wait until there’s an emergency to learn.
Storage and Expiration
Your injector won’t work if it’s been stored wrong.
- Keep it at room temperature - between 59°F and 86°F. Don’t leave it in a hot car or a freezing backpack.
- Protect it from light. Store it in its original case.
- Check the expiration date. Replace it every 18 months or when it expires - whichever comes first.
- Look at the liquid inside. If it’s cloudy, discolored, or has particles, throw it out and get a new one.
Even if it’s not expired, if it’s been through extreme heat or cold, it might not deliver the full dose. When in doubt, replace it.

What About Kids and Schools?
One in 13 children in the U.S. has a food allergy. That’s two kids in every classroom. Schools are required to have epinephrine on hand in 47 states - but only 28 states require staff to be trained.
If your child has a severe allergy, make sure:
- The school has at least two injectors on site.
- Teachers and nurses know where they are and how to use them.
- You’ve given them a written emergency plan.
- Your child wears a medical alert bracelet.
And don’t assume your child will know how to use it themselves. Even older kids often panic. Train the adults around them.
Cost and Access
Epinephrine auto-injectors are expensive. EpiPen costs around $680 without insurance. Adrenaclick is under $200. Auvi-Q is over $4,000 - but most people get it for free through patient assistance programs.
If cost is a problem, ask your doctor for samples. Many manufacturers offer coupons or free devices for low-income families. Some pharmacies have generic versions. Don’t skip having one because you think you can’t afford it. The cost of not having it? Unthinkable.
Final Warning: Don’t Delay
Dr. Robert Wood from Johns Hopkins says delaying epinephrine increases the chance of a second, deadlier reaction by 300%. That’s not a risk you take. Not when the alternative is death.
Epinephrine’s side effects - racing heart, shaking, feeling anxious - are scary. But they last less than 30 minutes. The symptoms of untreated anaphylaxis? They can last forever.
If you or someone you love has a serious allergy, you need to know this. Not just read it. Not just watch a video. Practice. Drill. Repeat. Keep the injector in your bag, your car, your desk. Make sure everyone who cares for your child knows how to use it.
Because when it matters most - when the airway closes, when the blood pressure drops - you won’t have time to think. You’ll only have time to act. And if you’ve practiced, you’ll act right.
Can you use an epinephrine auto-injector through clothing?
Yes. You can inject through jeans, leggings, or even thick pants. The needle is designed to pierce fabric. There’s no need to remove clothing during an emergency. This saves critical seconds and reduces the risk of contamination or exposure.
What if I accidentally trigger the injector?
If you accidentally press the tip and trigger the device, it will deliver a full dose into your finger or hand. This can cause local tissue damage and may require medical attention. Call 911 or go to the ER immediately. Do not try to remove the needle yourself. The risk of accidental activation is why you should always keep the safety cap on and store it securely.
Can you use someone else’s epinephrine injector?
Yes. If someone is having anaphylaxis and you have an injector - even if it’s not prescribed to them - give it. The dose is safe for adults and older children. It’s better to give a dose that’s slightly too high than to wait and risk death. Most states have Good Samaritan laws that protect you from liability if you act in good faith.
How long does epinephrine last in the body?
Epinephrine starts working within seconds and peaks in about 5 minutes. Its effects wear off after 10 to 20 minutes. That’s why a second dose may be needed if symptoms return. But the medicine doesn’t stay in your system for hours - it’s metabolized quickly. That’s also why hospital care is still required after use.
Is the nasal spray (Neffy) as good as the injection?
Neffy works for most people and is FDA-approved as an alternative. In clinical trials, it successfully treated 81% of severe reactions. But it requires proper technique: you must breathe in hard while spraying. In simulations, 32% of users failed to use it correctly. For people who are needle-averse, it’s a great option - but it’s not yet proven to be as reliable as an injection in real-world emergencies.
12 Comments
Danny Nicholls November 23 2025
I literally carried my kid's EpiPen in my fanny pack for 3 years 🎒❤️🩹. One time at the zoo, he ate a peanut butter cracker by accident and started turning red. I didn't even think-I just pulled it out, jabbed his thigh through his jeans, and held it like my life depended on it. (It did.) The voice on the Auvi-Q said 'Push firmly' like a calm robot mom. Best. Device. Ever.
Holly Schumacher November 23 2025
I can't believe people still think Benadryl is a substitute. This isn't a Pinterest post-it's a biological emergency. Epinephrine is the only thing that reverses histamine-induced vascular collapse. Antihistamines? They're for hives. Not for when your airway is being strangled by your own immune system. Stop romanticizing delay. People die because of this ignorance.
Robin Johnson November 25 2025
Practice on an orange. Seriously. I used to do it in the shower every Sunday night-right after brushing my teeth. One-handed. With jeans on. Eyes closed. My wife thought I was crazy. Then our daughter had her first reaction at school. The nurse used the EpiPen like she’d done it a hundred times. She had. Because I made sure she did.
Latonya Elarms-Radford November 26 2025
The tragedy of modern medicine is not the lack of innovation-it's the lack of embodied knowledge. We have devices that talk to us, yet we outsource survival to algorithms. Epinephrine is not a gadget-it is a covenant between the human body and the will to live. To treat it as a checklist item is to misunderstand the sacredness of breath. When the throat closes, it is not the needle that saves-it is the courage to act before the mind has time to question.
Michael Fitzpatrick November 27 2025
I used to think I’d panic if I had to use one. But after practicing with the trainer pen every few months, it became like buckling a seatbelt. No thought. Just action. I keep mine in my work bag, my car, and my wife’s purse. We even got a spare for the dog walker. You never know when you’ll be the person who has to be the calm one.
Shawn Daughhetee November 29 2025
my kid got stung by a wasp last summer and i was shaking so bad i dropped the epi pen twice but then i just closed my eyes and jammed it in his leg like the video said and it worked thank god
Justin Daniel November 30 2025
I’ve seen so many people stress about the needle. But here’s the thing-nobody remembers the sting after they’re breathing again. I got Neffy for my partner because they hate needles. We practiced with the demo spray for 2 weeks. Still, I keep an EpiPen too. Better safe than sorry. And yes, you can absolutely use someone else’s. If someone’s blue and gasping, don’t ask for ID. Just inject.
Melvina Zelee November 30 2025
i always thought epinephrine was for like doctors or something but then my cousin had a reaction at a birthday party and the mom just pulled out this little thing from her purse and jabbed it and it was like magic. i cried. now i have one in my purse and i tell everyone to get one. life is short and allergies are sneaky
steve o'connor December 2 2025
In Ireland we don’t have as many food allergies, but I’ve got an EpiPen in my backpack since my niece had that peanut reaction at a pub last year. The staff didn’t know what to do. I did. Because I read the damn guide. You don’t need to be a medic to save a life. Just be prepared.
ann smith December 4 2025
I'm a school nurse, and I've trained over 120 staff members on how to use these. The biggest mistake? Waiting. Waiting for permission. Waiting for symptoms to 'get worse.' Don't. Just. Wait. If in doubt-administer. Side effects are temporary. Death is permanent. I keep extra injectors in every classroom. It's not extra work. It's basic care.
Julie Pulvino December 4 2025
My son’s first reaction was at a birthday party. I didn’t even know he was allergic until then. We had the EpiPen, but I didn’t know how to use it. I called 911, panicked, and just held it. A stranger in the room grabbed it from me, pulled the cap, and jabbed him. He was fine. That stranger is now my hero. I practice with the trainer every month. You don’t need to be brave-you just need to be ready.
Patrick Marsh December 5 2025
Don't forget: remove the blue cap. Hold for 3 seconds. Inject thigh only. Call 911. Second dose if needed. Store at room temp. Replace expired ones. Practice monthly.