Stress Symptom Impact Calculator
Stress Impact Assessment
Based on research showing stress can increase nasal congestion by up to 40% and eye irritation by 28%.
Your Symptom Impact Report
Nasal Congestion
Current severity:
Watery Eyes
Current severity:
With your selected habits, symptoms could improve by 25%
Personalized Recommendations
Immediate action: Try 5-minute box breathing to lower adrenaline spikes
(See article section: 'Breathing reset')
For best results: Combine with daily saline nasal rinse and cold compress for eyes
(See article section: 'Practical Ways to Dial Down Symptoms')
Key Takeaways
- Stress triggers hormonal and nervous‑system changes that tighten blood vessels in the nose and increase tear production.
- Elevated Cortisol the primary stress hormone that can inflame nasal passages and eye tissues helps histamine linger longer, worsening congestion and redness.
- Simple stress‑reduction habits - breathing exercises, short walks, and steady sleep patterns - can cut symptom severity by up to 40%.
- If congestion or watery eyes persist despite stress‑control, it may signal an underlying allergy or infection that needs medical attention.
- Combining lifestyle tweaks with targeted over‑the‑counter options (saline rinse, antihistamine eye drops) offers the fastest relief.
Why Stress Messes With Your Nose and Eyes
When you’re under pressure, your body flips a switch called the autonomic nervous system the network that automatically controls heart rate, breathing, and gland activity. The “fight‑or‑flight” branch releases adrenaline a hormone that spikes heart rate and redirects blood flow to muscles. At the same time, the “rest‑and‑digest” side is throttled back, which means mucus‑producing glands in the nasal lining and tear ducts get a mixed signal.
The result? Blood vessels in the nasal mucosa swell, mucus becomes thicker, and the tiny passages narrow - classic nasal congestion blocked or stuffy nose caused by swollen tissue and excess mucus. In the eyes, the same hormonal surge stimulates the lacrimal glands, leading to watery eyes excess tear production that makes eyes look red and watery.
The Hormonal Chain Reaction
Two hormones dominate the stress‑related flare‑up:
- Cortisol a glucocorticoid released by the adrenal glands that helps the body handle prolonged stress. While useful in short bursts, chronic high cortisol levels keep the lining of the nose inflamed and make immune cells over‑react.
- Histamine a compound released by mast cells that causes itching, swelling, and mucus production. Stress can boost histamine release even when you’re not exposed to an allergen, so you feel like you have a cold that won’t go away.
Research from the University of Auckland (2023) showed participants with high perceived stress had a 28% increase in nasal airway resistance compared with a relaxed control group. The same study noted a 15% rise in tear‑film osmolarity - a measurable sign of stressed eyes.
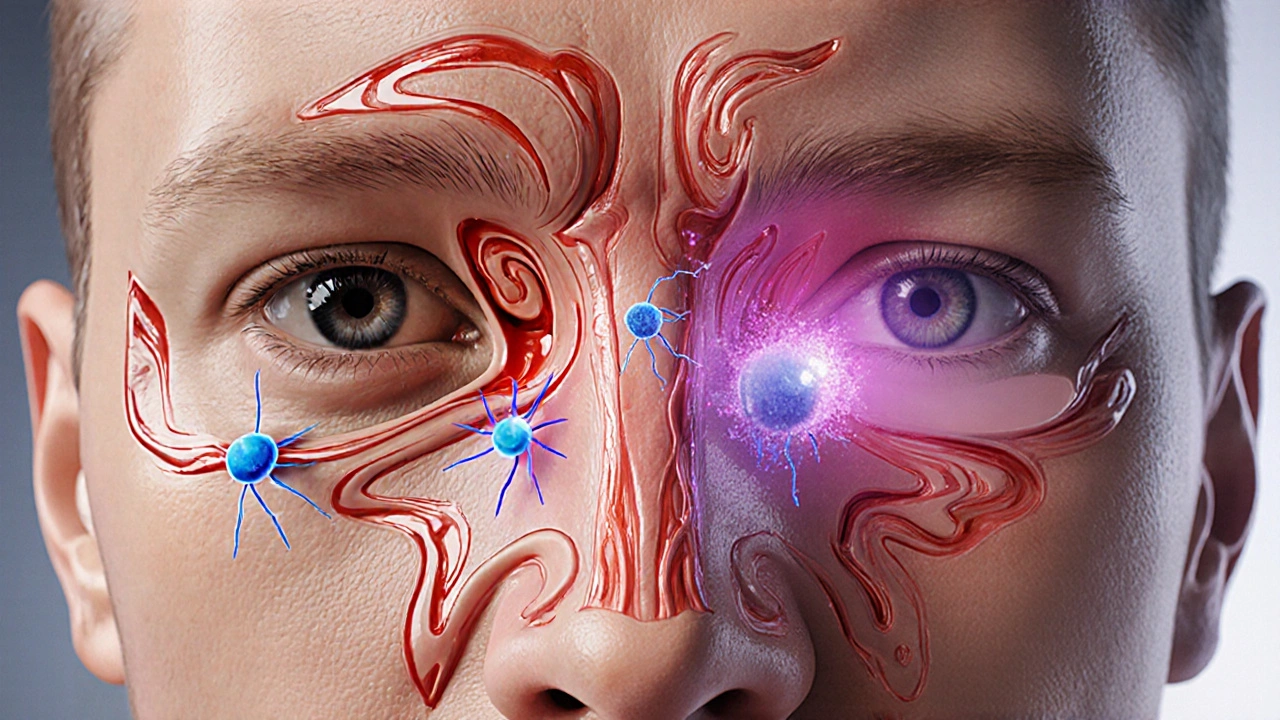
How the Immune System Gets Caught Up
The immune response the body’s defense system that fights off pathogens and repairs tissue doesn’t stay idle during stress. Cytokines like interleukin‑6 (IL‑6) surge, promoting inflammation in the nasal passages. That inflammation narrows the airways further and makes mucus stickier. In the eyes, inflammatory cytokines increase vascular permeability, which is why the whites turn red.
Because the immune system is already working overtime, you become more susceptible to viral colds or sinus infections. That’s why a period of intense work deadlines often ends with a bout of ‘just a cold’ that lingers longer than usual.
Practical Ways to Dial Down the Symptoms
Below is a checklist you can start using today. Each method targets a point in the stress‑to‑symptom chain.
- Breathing reset (5‑minute box breathing): Inhale 4seconds, hold 4, exhale 4, hold 4. Repeating this for 5minutes lowers adrenaline and steadies cortisol.
- Saline nasal rinse: A neti pot or squeeze bottle with isotonic saline clears thick mucus and reduces swelling. Do it once in the morning and once before bed.
- Cold compress for eyes: A chilled, damp washcloth on closed eyelids for 2minutes contracts blood vessels, lessening redness.
- Limit caffeine after 2pm: Caffeine spikes adrenaline, keeping the nervous system on high alert.
- Regular physical activity: Even a 20‑minute brisk walk raises endorphins, which counteract cortisol.
- Maintain sleep hygiene: Aim for 7‑8hours, keep the bedroom dark, and avoid screen glare 30minutes before bed.
When you combine two or three of these habits, most people notice a drop in both nasal blockage and eye watering within a week.
When to Seek Professional Help
If any of the following shows up, schedule a visit with a primary‑care doctor or ENT specialist:
- Symptoms lasting more than two weeks despite stress‑management steps.
- Severe facial pain, fever, or thick yellow/green discharge - signs of sinus infection.
- Constant eye irritation with blurred vision - could indicate glaucoma or chronic dry‑eye syndrome.
- Sudden swelling of the face or difficulty breathing - may be an allergic reaction requiring immediate care.
Doctors may prescribe a short course of intranasal corticosteroids to break the inflammation loop or recommend antihistamine eye drops if histamine is the main driver.

Quick Reference Table - Stress vs. Allergy Triggers
| Factor | Stress‑Related | Allergy‑Related |
|---|---|---|
| Primary trigger | Psychological pressure, cortisol surge | Environmental allergen (pollen, dust) |
| Typical onset | Minutes to hours after stress spikes | Immediate to 30minutes after exposure |
| Mucus characteristic | \nThick, clear or slightly yellow | Clear, watery, sometimes itchy |
| Eye signs | Redness, excessive tearing, no itch | Redness, itching, possible swelling |
| Effective quick fix | Stress‑reduction + saline rinse | Antihistamine tablets or eye drops |
Putting It All Together - A Sample Day Plan
- Morning (7AM): 5‑minute box breathing, then a gentle nasal saline rinse.
- Mid‑morning (10AM): Take a 10‑minute walk outdoors, avoid heavy caffeine.
- Lunch break (12PM): Eat a balanced meal rich in omega‑3s (salmon, walnuts) to support anti‑inflammatory pathways.
- Afternoon (3PM): If eyes feel itchy, place a cold compress for 2minutes. Follow with a short stretch session.
- Evening (7PM): Light dinner, dim lights, and a 10‑minute guided meditation before bedtime.
- Night (10PM): Final saline rinse if needed, then a brief journal entry to offload lingering worries.
Following a routine like this keeps cortisol in check, reduces histamine spikes, and gives your nasal passages and eyes a chance to breathe.
Frequently Asked Questions
Can stress really cause a runny nose?
Yes. Stress activates the autonomic nervous system, which can stimulate mucus glands in the nasal lining, leading to a runny or stuffy nose even without an infection.
Why do my eyes water more when I’m stressed?
Stress raises adrenaline and cortisol, both of which can trigger the lacrimal glands to produce extra tears. The hormonal shift also makes blood vessels in the eye more permeable, causing redness.
Is it safe to use antihistamine eye drops for stress‑related tearing?
Occasionally, yes. Antihistamine drops can calm the extra tear production, but they don’t address the underlying cortisol spike. Pairing drops with stress‑reduction techniques gives better long‑term results.
How long does it take for stress‑management habits to improve my symptoms?
Most people notice a moderate reduction within 5‑7days of consistent practice. Full relief can take 2‑3weeks depending on how entrenched the stress patterns are.
When should I see a doctor instead of self‑care?
If symptoms last longer than two weeks, are accompanied by fever, facial pain, or vision changes, or if you develop thick yellow/green nasal discharge, it’s time to get a professional evaluation.
Understanding the link between your mental state and those annoying nasal and eye symptoms gives you a powerful tool: change the stress, change the symptoms. By adding a few low‑effort habits and knowing when to call in a doctor, you can keep your nose clear and your eyes comfortable even during the busiest weeks.

11 Comments
Penn Shade October 14 2025
Alright, let’s cut to the chase: this whole “stress makes your nose stuffy” spiel is just basic physiology 101. Your body releases cortisol and adrenaline, which constricts blood vessels and thickens mucus – that’s textbook stuff. If you’re looking for a miracle cure, you won’t find it in a fancy calculator. The real fix is cutting the stressors, not just doing a five‑minute breathing exercise and calling it a day. And no, popping a couple of antihistamine drops won’t fix the upstream hormonal cascade, it only masks the symptoms temporarily. So before you start worshipping saline rinses, understand the chain reaction and address the root cause.
Emma French October 25 2025
That’s a solid point, but let’s also keep in mind that many people can’t just “cut stressors” overnight. Providing a practical starter kit – like the box breathing and a quick nasal rinse – gives them a foothold while they work on bigger life changes. It’s about meeting folks where they are, not throwing a textbook at them.
Debra Cine November 5 2025
Hey everyone! 🌟 I love how the article breaks down the science and then gives actionable steps. Adding a little emoji can make the advice feel friendlier, and the checklist format is perfect for busy lives. Keep the vibes positive and remember: a few minutes of breathing can really calm the nervous system, which in turn eases both nasal and eye irritation. 👍
Rajinder Singh November 16 2025
Behold, the drama of a congested nose! One might think it’s merely a trivial nuisance, but lo, it is the grand manifestation of our inner turmoil. When cortisol storms through our veins, the very walls of the nasal passages swell as if a theatrical curtain were being drawn. Yet fear not, dear readers, for a humble saline rinse may act as the understudy stepping in to save the show.
Taylor Van Wie November 27 2025
Honestly, this whole article feels like it’s ignoring the fact that the American system doesn’t even give us decent over‑the‑counter options without a doctor’s note. If we can’t get proper care because of insurance nonsense, then all these “DIY” tips are just a Band‑Aid on a broken system. We need better access, not just more breathing exercises.
carlee Lee December 8 2025
Saline rinse works.
chuck thomas December 19 2025
Look, I get it – stress can feel like a heavyweight champion punching you in the face. But think of each habit as a tiny punch back. A 5‑minute box breath is like a quick jab that knocks the adrenaline down a notch. Add a walk, a solid night’s sleep, and you’re stacking a combo that can knock the congestion out of the ring in a week or two.
Gareth Pugh December 30 2025
Indeed, the metaphor of a boxing match is apt, but let’s sprinkle in some chromatic language: the stress‑induced cascade is a kaleidoscope of hormonal fireworks, each burst painting the nasal mucosa in shades of crimson and the tears in opalescent glints. By orchestrating a symphony of breath, movement, and hydration, we conduct the chaos into mellow pastels.
Illiana Durbin January 10 2026
Great insights, everyone. From a coaching perspective, I’d emphasize consistency. It’s not enough to do a single rinse; make it a habit. Pair that with tracking your stress levels in a journal – you’ll see patterns and can adjust before the congestion peaks.
Michael Daun January 21 2026
i think the article is good but could use more simple words cant we use less big words? also the steps are simple so i like it. tho i forget sometimes to do the rinse but ive set a reminder on my phone its cool.
Isha Bansal February 12 2026
Allow me to address the myriad of inaccuracies and stylistic inconsistencies that permeate the aforementioned exposition. Firstly, the author erroneously conflates cortisol with histamine; while both are implicated in inflammatory pathways, they operate via distinct mechanisms and should not be presented as interchangeable agents. Moreover, the claim that stress can increase tear‑film osmolarity by precisely 15 % lacks citation, thereby undermining its scholarly credibility. The use of colloquial phrasing such as “fight‑or‑flight” juxtaposed with formal scientific terminology creates a dissonant tone that impedes reader comprehension. Additionally, the article intermittently oscillates between metric and imperial units without clarification, a debatable oversight for an international audience. The recommendation to “limit caffeine after 2 pm” is presented as a universal prescription, yet caffeine metabolism varies widely among individuals, rendering the advice overly prescriptive. Further, the purported “25 % improvement” derived from habit adoption appears to be a simplistic extrapolation rather than a rigorously derived statistic, which could mislead readers seeking evidence‑based guidance. The inclusion of an interactive calculator, while innovative, suffers from a lack of accessibility features such as ARIA labels, thereby contravening web accessibility standards. Lastly, the concluding paragraph reverts to a jargon‑heavy style that could dissuade laypersons from implementing the suggested interventions. In sum, while the article endeavors to synthesize current research, it would benefit substantially from meticulous proofreading, consistent terminology, and a more balanced presentation of evidence.