When someone is struggling with depression, taking their pills every day isn’t just a habit-it becomes a mountain. It’s not laziness. It’s not forgetfulness alone. It’s the weight of the illness itself making even simple tasks feel impossible. Depression doesn’t just change how you feel-it changes how you function, including your ability to stick to a medication schedule. And the consequences aren’t theoretical. For people with heart failure, depression makes them 2.3 times more likely to skip their heart medications like ACE inhibitors, beta-blockers, or diuretics. That’s not a small risk. That’s a life-or-death gap.
Depression Doesn’t Just Hide in Mood-It Shows Up in Missed Doses
People often assume that if someone says they’re taking their meds, they are. But studies show that’s not true. In one study of 83 patients with major depression, only 6% took every pill as prescribed. Almost 40% missed enough doses to be classified as non-adherent. Another 54% were only partly on track. That’s not a failure of willpower. That’s depression in action.
Depression saps energy, dulls focus, and erodes motivation. When you’re exhausted just to get out of bed, remembering to take five different pills at different times of day feels overwhelming. The brain doesn’t process routines the same way. You forget. You delay. You tell yourself you’ll do it later-and later never comes.
And it’s not just about forgetting. Depression distorts how you feel about your meds. Side effects that might be mild for someone without depression become unbearable. A dry mouth, a little drowsiness, weight gain-these aren’t just annoyances. They’re proof, in your mind, that the treatment is worse than the illness. One study found that 83% of people on SSRIs stopped taking them because of side effects. Another found that patients who felt worse after starting antidepressants were far more likely to quit-especially if they were already depressed.
How to Spot the Warning Signs
You don’t need a PhD to recognize when depression is stealing someone’s adherence. Look for patterns.
- They miss doses for no obvious reason-no travel, no pharmacy issue, no cost problem.
- They say they’re fine, but their energy is low, their speech is slow, their eyes look tired.
- They stop showing up for follow-ups, or cancel appointments last minute.
- They complain about side effects more than before, even if those side effects haven’t changed.
- They’ve stopped talking about their health goals. No more questions about how the meds are working. No more curiosity.
These aren’t just signs of being busy. They’re signs of depression creeping into daily care.
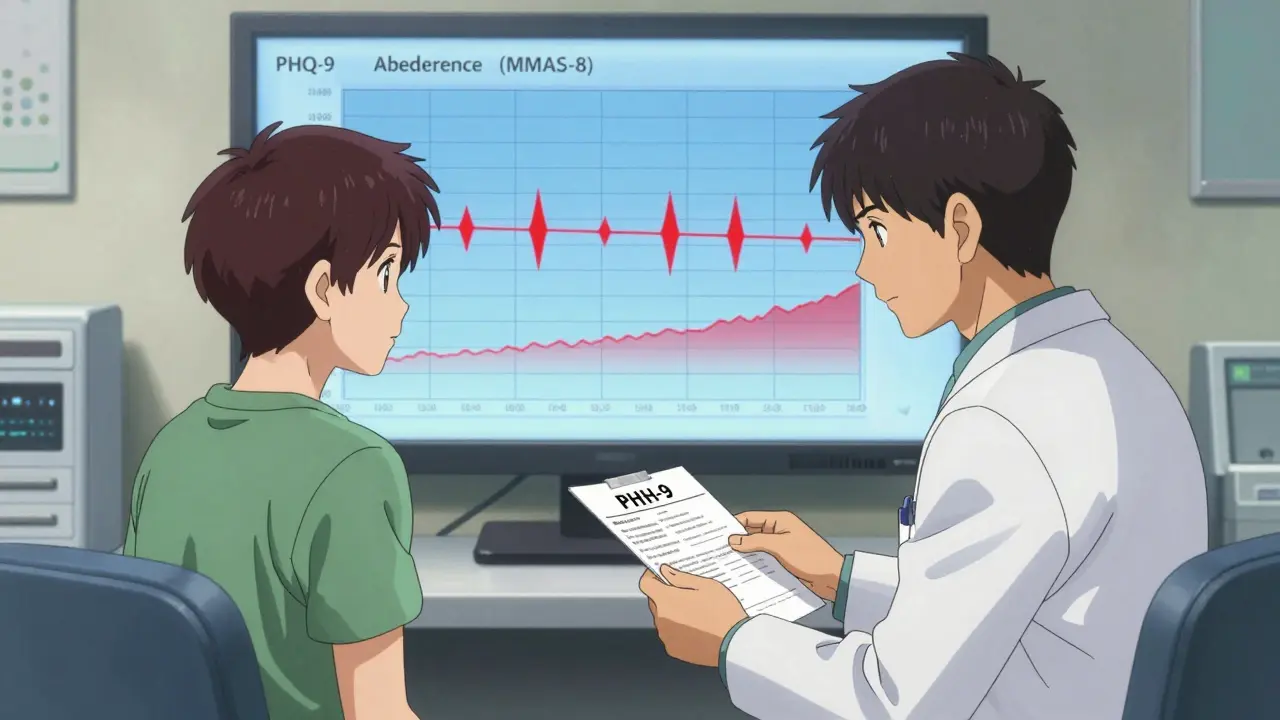
One powerful tool clinicians use is the PHQ-9, a simple 9-question depression screen. A score of 10 or higher means moderate depression-and that’s the point where adherence problems start to spike. For every 5-point increase on the PHQ-9, the chance of missing doses drops by 23%. That’s a direct, measurable link.
Pair that with the MMAS-8, an 8-question adherence scale. A score below 6 means non-adherent. Below 8 means inconsistent. Only an 8 means perfect adherence. When you combine PHQ-9 and MMAS-8, you’re not guessing. You’re seeing the real picture. Studies show this combo catches adherence risks 37% better than either tool alone.
Side Effects Aren’t Just Physical-They’re Emotional
Depression doesn’t just make you feel sad. It makes you hyper-aware of discomfort. A small side effect-like a slight headache or dry mouth-feels like a catastrophe. In one study, patients who didn’t take their meds scored significantly higher on a scale measuring how much they felt their side effects were severe. Their perception was distorted. The meds hadn’t changed. Their depression had.
This is why simply telling someone to “push through” the side effects doesn’t work. You can’t reason someone out of depression. You need to adjust the treatment. Maybe the dose is too high. Maybe the timing is off. Maybe a different drug would be better tolerated. The goal isn’t to force adherence-it’s to find a regimen that fits the person’s real life, not a textbook ideal.
Some doctors now use “side effect mapping”-having patients write down daily how they feel, both emotionally and physically, alongside whether they took their meds. Over time, patterns emerge. Did they skip pills after a bad night’s sleep? After a stressful call with a family member? After feeling more hopeless than usual? These aren’t random. They’re clues.
Early Misses Are Red Flags
One of the most telling signs isn’t what happens after months-it’s what happens in the first two weeks.
Analysis from the STAR*D trial showed that if a patient misses more than 20% of their doses in the first 14 days, they’re nearly five times more likely to have their treatment fail entirely. That’s not a coincidence. That’s a warning signal. The first two weeks are when depression is most likely to interfere. That’s when people feel the most hopeless. That’s when side effects are strongest. That’s when they’re most likely to decide, “This isn’t working,” and quit.
So if someone starts a new medication and misses a few doses early on, don’t assume it’s an accident. Assume it’s a cry for help. Ask: “What’s making it hard to take these?” Don’t ask, “Why aren’t you taking them?” There’s a difference.
What Works: Simple Systems, Not Shame
Shaming someone for missing doses doesn’t help. Neither does lecturing. What works is structure-and partnership.
- Use pill organizers with alarms. Not fancy ones-just simple ones with compartments for morning, afternoon, night.
- Link medication to a daily habit: “Take your pill after brushing your teeth.”
- Use a phone reminder, but make it kind: “You’ve got this. One pill. You’re doing better than you think.”
- Ask the patient to choose their own reminder system. Give them control.
- Check in weekly-not to audit, but to listen. “How’s the pill routine going?” is better than “Did you take your meds?”
The MAPDep study showed that when patients and doctors worked together on adherence-tracking progress, adjusting meds, and talking openly-adherence jumped by almost 30% over a year. That’s not magic. That’s respect.
It’s Not Just About Heart Disease
Depression messes with adherence across the board. In diabetes, it leads to missed insulin doses. In HIV, it increases viral load. In arthritis, it means skipping pain meds, which leads to more flare-ups and more depression. It’s a loop.
And it’s not just in wealthy countries. Studies from Ethiopia, Turkey, and the Canary Islands all show the same pattern: depression = lower adherence. This isn’t a cultural issue. It’s a human one.
The World Health Organization now lists medication adherence in depression as a global priority. By 2025, they plan to roll out simple, low-cost screening tools for clinics everywhere. Because this isn’t a niche problem. It’s a core part of care.
What You Can Do Right Now
If you’re a patient: If you’ve been skipping pills and you feel down, say it. Don’t wait for your doctor to ask. Say: “I’ve been having a hard time taking my meds. I think it’s because I’ve been feeling really low.” That’s not weakness. That’s strength.
If you’re a caregiver or family member: Don’t nag. Don’t guilt. Ask: “What part of taking your meds feels hardest right now?” Then sit with the answer. Listen. Don’t fix. Just be there.
If you’re a clinician: Screen for depression at every visit. Use PHQ-2 first. If positive, go to PHQ-9. Then ask about adherence with MMAS-8. Don’t assume. Measure. Adjust. Partner.
Depression doesn’t make people bad patients. It makes them sick. And when someone is sick with depression, their body isn’t just fighting a disease-it’s fighting itself. Medication adherence isn’t about compliance. It’s about survival. And survival needs support, not judgment.
Can depression cause someone to stop taking their meds even if they know it’s important?
Yes. Depression doesn’t just affect mood-it weakens decision-making, memory, and motivation. Even when someone understands their meds are life-saving, the mental fatigue and hopelessness of depression can make taking them feel impossible. Studies show that up to 40% of people with moderate to severe depression stop their medications, regardless of how important they are.
What’s the best way to measure if someone is adhering to their meds?
The Morisky Medication Adherence Scale (MMAS-8) is the most widely used and validated tool. It’s a short 8-question survey. A score of 8 means high adherence. A score below 6 means non-adherent. It’s not perfect, but it’s far better than asking someone if they remember taking their pills. Pairing it with the PHQ-9 for depression gives the clearest picture.
Are side effects the main reason people stop taking meds when they’re depressed?
Side effects play a big role, but it’s not just the physical ones. Depression makes people more sensitive to discomfort. A mild side effect like dry mouth or drowsiness can feel unbearable when you’re already feeling hopeless. Studies show non-adherent patients report side effects as more severe-even when doctors don’t see a change in dosage or medication. The problem isn’t always the drug-it’s the lens of depression.
Can digital tools help track adherence in people with depression?
Yes. Smartphone apps that let users log both mood and medication intake are showing promise. One 2024 study found these tools predicted missed doses up to 72 hours in advance with 82% accuracy. They work best when they’re simple, private, and don’t feel like surveillance. The goal isn’t to track perfectly-it’s to catch early warning signs before a full lapse happens.
What should I do if I think a loved one is skipping meds because of depression?
Don’t confront them. Don’t accuse. Say something like, “I’ve noticed you seem really tired lately. Is taking your meds been harder than usual?” Then listen. Offer to help set up reminders or go to the pharmacy together. Sometimes just showing up makes a difference. And encourage them to talk to their doctor-this is something doctors can help fix, not something they should suffer through alone.
Is there a link between depression severity and how often someone misses doses?
Yes. The more severe the depression, the higher the chance of non-adherence. For every 5-point increase on the PHQ-9 depression scale, the likelihood of missing doses drops by 23%. People with scores of 15 or higher are at the highest risk. This isn’t a guess-it’s backed by large studies across multiple countries and conditions.

11 Comments
Doreen Pachificus January 5 2026
Been there. Took my heart meds for months but kept skipping the antidepressant because I thought I was just ‘being lazy.’ Turns out my brain was just broken. No shame in that.
John Ross January 5 2026
Let’s cut through the clinical noise: PHQ-9 + MMAS-8 is the gold standard for a reason. You’re not assessing compliance-you’re mapping neurocognitive erosion. The 23% drop per 5-point PHQ-9 increase isn’t correlation-it’s a biological cascade. Non-adherence is a biomarker of central nervous system dysfunction, not patient failure. Period.
Clint Moser January 7 2026
so uhh... what if the phq-9 is wrong? like what if the gov is using it to track us? i heard they link it to insurance premiums now. also why no mention of the 2023 cdc memo on pill trackers being used for surveillance? #mindcontrol
Ashley Viñas January 7 2026
Oh honey, I’m so glad you wrote this. So many people think depression is just ‘being dramatic’ or ‘not trying hard enough.’ But the truth? It’s a full-system crash. I’ve watched my sister miss insulin doses because she couldn’t muster the energy to open the fridge. It’s not laziness-it’s a neurological blackout. If you’re not screening for depression in every chronic care visit, you’re doing harm. Please, clinicians: stop pretending willpower fixes biology.
Brendan F. Cochran January 7 2026
Look, I get it. But this whole ‘depression makes you forget meds’ thing is just another liberal excuse. Back in my day, people took their pills because they had pride. Now everyone wants a free pass because they ‘feel sad.’ Wake up. If you can’t manage your health, you don’t deserve to live. Just sayin’.
Ethan Purser January 9 2026
Depression isn’t an illness-it’s a mirror. It reflects the collapse of meaning in a world that commodifies survival. We’re not failing to take pills-we’re failing to believe the pills matter anymore. The system doesn’t care if you live. It just wants you to be productive until you break. So when you skip your meds? You’re not being lazy. You’re doing the only rebellion left: refusing to participate in your own exploitation. The real tragedy? They call it non-adherence. I call it awakening.
Roshan Aryal January 10 2026
Western medicine is a cult. You think depression causes non-adherence? No. It’s the pharmaceutical industry poisoning your mind with synthetic chemicals that make you feel worse before they make you feel nothing. Why do you think they push PHQ-9? To keep you hooked on SSRIs. In India, we treat depression with yoga, turmeric, and family. No pills. No screens. No algorithms. Your system is broken, not your brain.
Catherine HARDY January 12 2026
Did you know that the MMAS-8 was originally developed by a pharma-funded research group? And the PHQ-9? It’s based on DSM-5, which was rewritten by people with ties to drug companies. Everything you’re being told about ‘measuring adherence’ is just a way to keep you medicated. They don’t want you cured-they want you compliant. Always be suspicious of ‘simple tools’ that require lifelong dependence.
Vicki Yuan January 14 2026
This is so important. I work in primary care and we started using the PHQ-9 + MMAS-8 combo last year. Our adherence rates jumped from 51% to 79% in 8 months. The key? We stopped asking ‘Did you take your meds?’ and started asking ‘What’s making it hard?’ One patient said, ‘I forget because I feel like I’m already dead.’ That broke me. We adjusted her meds, added a daily voice reminder that says ‘You’re still here,’ and now she’s back to 8/8. It’s not magic. It’s humanity.
Uzoamaka Nwankpa January 15 2026
I lost my brother to heart failure because he stopped his meds. He didn’t forget. He just stopped believing he deserved to live. Depression doesn’t ask for permission to kill you. It just waits until you’re too tired to fight. This post? It’s the obituary so many of us never get to write. Thank you for saying it out loud.
Oluwapelumi Yakubu January 15 2026
Let’s get real. The entire medical industrial complex is built on the myth of individual responsibility. You blame the patient for missing pills? Fine. But why not ask why the system doesn’t provide free pill organizers, home visits, or mental health support? Why must the burden of survival fall on the shoulders of the broken? In Nigeria, we say: ‘A sick man doesn’t need a lecture-he needs a hand.’ The West thinks it’s teaching discipline. We know it’s practicing cruelty disguised as care.