Automated Dispensing Cabinets (ADCs) are everywhere in modern clinics. They look like high-tech lockers, beep when you scan a badge, and hand out pills with a barcode click. Sounds simple, right? But here’s the truth: ADCs don’t prevent medication errors-they just change how they happen. A well-run ADC cuts errors by up to 50%. A poorly set up one? It can make them worse. In fact, one study found that in six out of seven nursing units, errors went up by more than 30% after ADCs were installed. Why? Because these machines aren’t magic. They’re tools. And tools used without understanding can hurt more than help.
What Exactly Is an ADC, and Why Does It Matter?
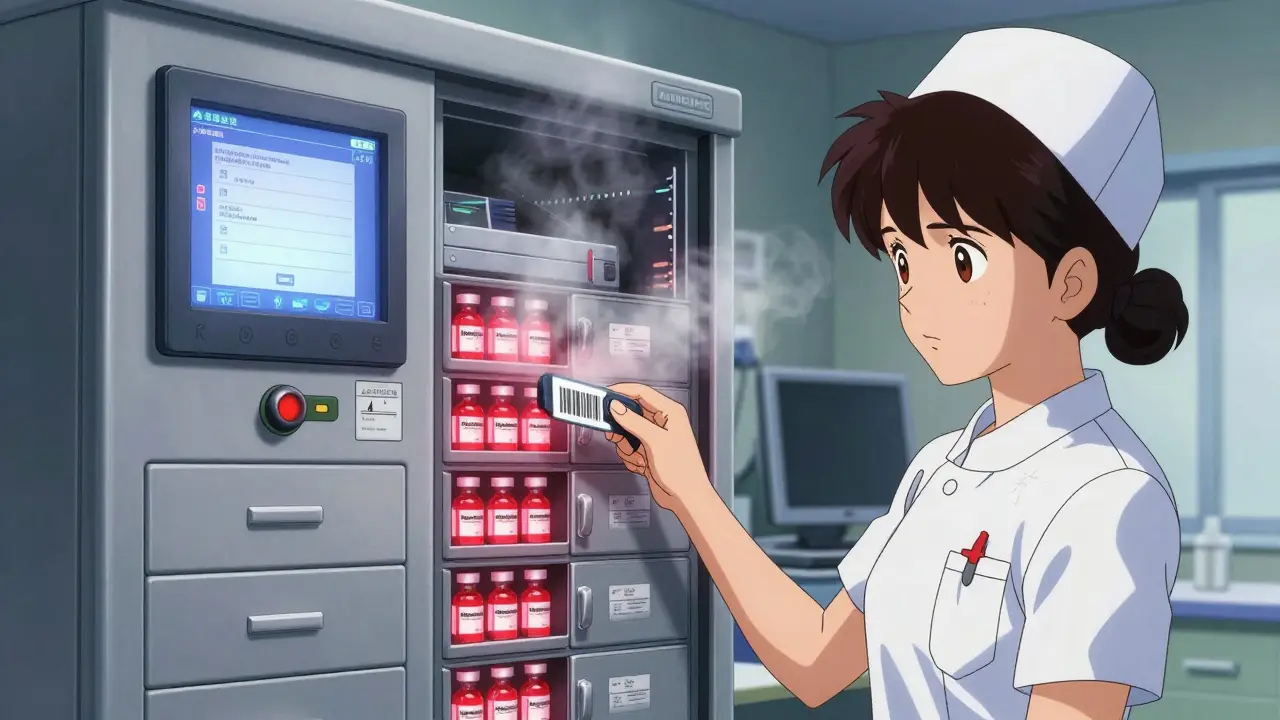
An Automated Dispensing Cabinet (ADC) is a computer-controlled storage system for medications. It replaces old metal drawers and rolling carts. Instead of nurses walking to the pharmacy for every dose, they pull pills right from the unit on their floor. Systems like BD Pyxis, Omnicell XT, and Capsa NexsysADC are common. They connect to your hospital’s electronic health record (EHR), track who took what, when, and why. They lock down dangerous drugs-like fentanyl, insulin, or morphine-so only authorized people can access them. Temperature-controlled zones keep refrigerated meds safe. Barcode scanning ensures the right drug goes to the right patient.
But here’s the catch: ADCs were never meant to replace pharmacist oversight. They were built to speed up access while keeping a digital paper trail. The problem? Many clinics treat them like vending machines. Nurses rush. Overrides get used too often. Drugs get stored next to look-alike, sound-alike ones. And no one checks if the cabinet even knows what’s inside.
The Nine Rules for Safe ADC Use (From the Experts)
In 2019, the Institute for Safe Medication Practices (ISMP) released nine Core Safety Processes. These aren’t suggestions. They’re the bare minimum for keeping patients safe. If your clinic skips even one, you’re playing Russian roulette with medication errors.
- Environmental setup - Don’t put the cabinet near a heater, sink, or window. Heat and moisture ruin pills. Keep it away from monitors-heat from screens can affect drug stability.
- User access - Only trained staff should log in. Passwords must be unique. No shared logins. Biometrics (fingerprint or facial scan) are better than passwords.
- Medication placement - Keep look-alike drugs far apart. Insulin should never sit next to heparin. Fentanyl should not be in the same drawer as naloxone. One nurse on Reddit said she scanned fentanyl thinking it was naloxone-caught it just in time. That was luck. Don’t rely on it.
- Barcode scanning - Every time you take a drug, scan the patient’s wristband AND the medication. No exceptions. If the system says “mismatch,” stop. Don’t override unless it’s an emergency-and even then, document why.
- Restocking control - Only pharmacists should load the cabinet. Nurses shouldn’t be adding meds. If they do, errors spike. A 2021 audit found 58% of clinics had this problem.
- Override limits - Overriding the system (bypassing safety checks) should be rare. Set daily limits per user. Require a second person to witness overrides. Document the reason. No “just in case” overrides.
- Drug configuration - The cabinet should block unsafe doses. If someone tries to pull 100mg of a drug that should be 10mg, it should refuse. This needs pharmacy input. Don’t let IT set it up alone.
- Temperature control - Refrigerated meds need labels with beyond-use dates. Store them away from electronics. Heat from the screen can make insulin break down faster.
- Staff training - New staff need 4-6 weeks of hands-on practice. Not a 20-minute video. Not a handout. Real practice. With supervision. Competency checks every year.

Why Your ADC Might Be Making Things Worse
Here’s what goes wrong in real clinics:
- Overuse of overrides - Nurses hit “override” because the system is slow. Or because they think they know better. Or because they’re tired. One facility had 47 overrides in a single shift. That’s not efficiency-that’s chaos. Facilities with no override controls had 2.3 times more errors.
- Wrong meds in the wrong drawer - A pharmacy restocked hydromorphone in the drawer labeled “morphine.” No one caught it. The patient got 3x the dose. They didn’t survive.
- No integration with the EHR - If the ADC doesn’t talk to the patient’s chart, it won’t warn you about allergies, duplicates, or interactions. You’re flying blind.
- Poor ergonomics - If the cabinet is too high, too low, or too far from the bed, nurses bend, stretch, and rush. One survey found 31% of pharmacists had back pain from ADC use. Pain leads to mistakes.
- Untrained staff - You wouldn’t let someone drive a car without a license. Why let them use a life-critical drug system with 15 minutes of training?
Mayo Clinic fixed this by creating unit-specific override lists. Only certain drugs could be overridden on certain floors. Result? A 63% drop in override-related errors. That’s not luck. That’s design.

What You Need to Do Right Now
If you run a clinic or manage one, here’s your checklist:
- Get your pharmacy team in charge - They need to design the cabinet layout, set up alerts, and approve every drug loaded. Not IT. Not nursing leadership. Pharmacy.
- Map your high-risk drugs - List the top 10 most dangerous meds you use. Make sure they’re spaced apart. Use color-coded labels. Put insulin in its own locked drawer with a separate barcode.
- Lock down overrides - Limit them to 2 per nurse per shift. Require a second licensed provider to witness every override. Document the reason in the EHR.
- Train like your life depends on it - Run mock drills. Give nurses a scenario: “The patient needs morphine. The system says ‘barcode mismatch.’ What do you do?” Don’t let them guess. Practice the answer.
- Check the temperature - Put a thermometer in the refrigerated drawer. If it’s above 8°C, it’s unsafe. Label every refrigerated med with a beyond-use date. Update it weekly.
- Do a monthly audit - Randomly check 5 cabinets. Is the barcode scanner working? Are look-alike drugs separated? Are override logs being reviewed?
What the Future Holds
ADCs are getting smarter. Omnicell’s new AI system flags suspicious patterns-like a nurse pulling 10 doses of fentanyl in 20 minutes. BD Pyxis now checks returned meds with barcode scans to catch wrong returns. Voice-controlled cabinets are coming in 2024. Biometric locks are rolling out in 2025.
But tech won’t save you. People will. The same mistakes that happened in 2017-wrong dose, wrong drug, no double-check-are still happening today. Because the tools are there. The training isn’t.
The goal isn’t to use the cabinet faster. It’s to use it smarter. Every beep, every scan, every override should be intentional. Not automatic. Not rushed. Not assumed.
Medication safety isn’t about machines. It’s about culture. If your clinic treats the ADC like a vending machine, it’ll treat your patients like an afterthought.
Can nurses restock Automated Dispensing Cabinets themselves?
No. Only licensed pharmacists should restock ADCs. When nurses or technicians add meds, errors jump. A 2021 ISMP audit found that clinics allowing non-pharmacists to restock had 40% more wrong-drug errors. Pharmacists are trained to spot look-alike/sound-alike drugs, check expiration dates, and confirm dosing. Letting others do it removes that safety layer.
What’s the biggest mistake clinics make with ADCs?
The biggest mistake is treating the ADC like a black box. They install it, assume it’s safe, and never check how it’s configured. They don’t review override logs. They don’t audit drug placement. They don’t train staff on what the alerts mean. An ADC without ongoing oversight is worse than no ADC at all.
Do ADCs really reduce medication errors?
Yes-but only if they’re set up right. Studies show ADCs can reduce dispensing errors by 15-20% compared to manual systems. But when poorly configured, they can increase errors by over 30%. The difference? Pharmacy involvement, barcode scanning, override limits, and staff training. Without those, the machine just automates mistakes.
How often should ADCs be audited?
At least once a month. Audits should check: barcode scanner function, drug placement (especially look-alike pairs), temperature logs, override frequency, and restocking logs. Some clinics do weekly audits on high-risk units like ICU or oncology. The Joint Commission expects documentation of these audits as part of medication safety standards.
What’s the cost of a single ADC unit?
Prices vary by size and features. A full-size unit like the Omnicell XT costs $25,000-$45,000. Smaller countertop models like Capsa’s 4T system run $15,000-$35,000. But the real cost isn’t the machine-it’s the training, audits, and staff time needed to keep it safe. A poorly managed ADC can cost far more in patient harm and liability.
Are ADCs used in ambulatory clinics too?
Yes, but less commonly. Only 42% of ambulatory clinics use them, compared to 98% of hospitals. Smaller clinics often use them for controlled substances or high-cost meds. The newer countertop models like Capsa’s 4T are designed for this. But even in small settings, the same safety rules apply: barcode scanning, pharmacist oversight, and override limits.
What should I do if I notice a drug is missing or mislabeled in the ADC?
Stop. Don’t use it. Report it immediately to pharmacy. If you’re unsure what’s supposed to be there, check the pharmacy’s master list or the cabinet’s digital inventory log. Never guess. A single mislabeled drug can lead to a fatal error. In 2017, a patient died after receiving 10 times the correct insulin dose because the ADC label was wrong. That mistake was caught too late.
Do ADCs work with all electronic health records?
Most modern ADCs connect via HL7 or FHIR standards, which most EHRs support. But compatibility isn’t guaranteed. Always confirm integration before purchase. If the ADC doesn’t talk to the EHR, it can’t check for allergies, duplicate therapy, or drug interactions. That’s like driving without a dashboard. You might get somewhere-but you won’t know if you’re in danger.
9 Comments
Brad Ralph February 13 2026
ADCs aren't magic. They're just expensive vending machines with a 20-minute training video. I've seen nurses override 12 times in one shift because the system "lagged." Lagged. Like it's 2005. We're automating human error, not fixing it.
Sophia Nelson February 15 2026
I work in a 40-bed unit. Our ADC has 37 overrides logged last week. No one was disciplined. No one even asked why. We're not managing safety-we're just documenting chaos.
Vamsi Krishna February 16 2026
Look, I've been in Indian ICUs where we used to hand-write med sheets on napkins. Now we got these fancy cabinets and still mess up? It's not the machine. It's the people who think the beep means "all good." My cousin died because the cabinet gave her morphine instead of fentanyl. Same drawer. Same barcode. Same arrogance. No one checks. No one cares. Until it's too late.
Annie Joyce February 18 2026
I'm a pharmacy tech and I can't believe how many units let nurses restock. Like, seriously? You wouldn't let a barista refill your insulin vial, right? Pharmacists are trained to catch look-alikes. A nurse rushing to get meds for a Code Blue? They're not looking at labels-they're looking at the clock. And that's when the wrong drug slips in. I've seen it. Twice. Both times, the patient lived. One didn't.
Stephon Devereux February 19 2026
The real problem? We treat ADCs like they're supposed to think for us. They're not. They're mirrors. They reflect your culture. If your unit is chaotic, the ADC becomes chaos with a screen. If your team trains like it matters, the ADC becomes a shield. It's not about the tech. It's about the daily ritual of double-checking, questioning, and owning the outcome. Stop blaming the machine. Start owning the process.
Carla McKinney February 21 2026
The ISMP guidelines? Cute. But let's be real: 87% of hospitals don't even have a dedicated pharmacist on the ADC committee. The rest are just IT guys with a PowerPoint. You can't fix human failure with a barcode scanner. You need accountability. You need consequences. You need someone to lose their job when they override without documenting. But no-everyone gets a participation trophy. And patients pay the price.
Suzette Smith February 21 2026
I think we're overcomplicating this. My hospital uses ADCs and we've had zero errors in 3 years. Maybe it's because we just trust our nurses? Maybe the real issue is that we don't trust people anymore? Maybe the system is the problem, not the people?
andres az February 23 2026
You know what's really going on? The ADC manufacturers pay hospitals to install them. Then they sell the "audit software" as a separate $200k add-on. That's why no one audits. That's why overrides are ignored. That's why training is 15 minutes. This isn't about safety. It's about corporate profit. The machine isn't flawed. The whole system is rigged.
steve sunio February 25 2026
i dont think u understand. the real issue is not the adc. its the fact that nurses are overworked and understaffed. if u had 12 patients and 10 mins to get meds, u wud override too. its not the machine. its the system. stop blaming the tool. fix the work environment first. 🤷♂️