When someone suffers a severe injury-car crash, fall, gunshot wound-the biggest killer in the first hour isn’t the injury itself. It’s bleeding. Not the kind you see on TV, where blood spurts dramatically. It’s the quiet, internal bleeding that steals oxygen from organs, drops blood pressure, and shuts down the body before help arrives. For decades, doctors had few tools to stop it. Then came tranexamic acid.
What tranexamic acid actually does
Tranexamic acid isn’t a miracle drug. It doesn’t seal wounds or rebuild tissue. What it does is simpler, smarter, and surprisingly old-fashioned. It stops clots from falling apart.
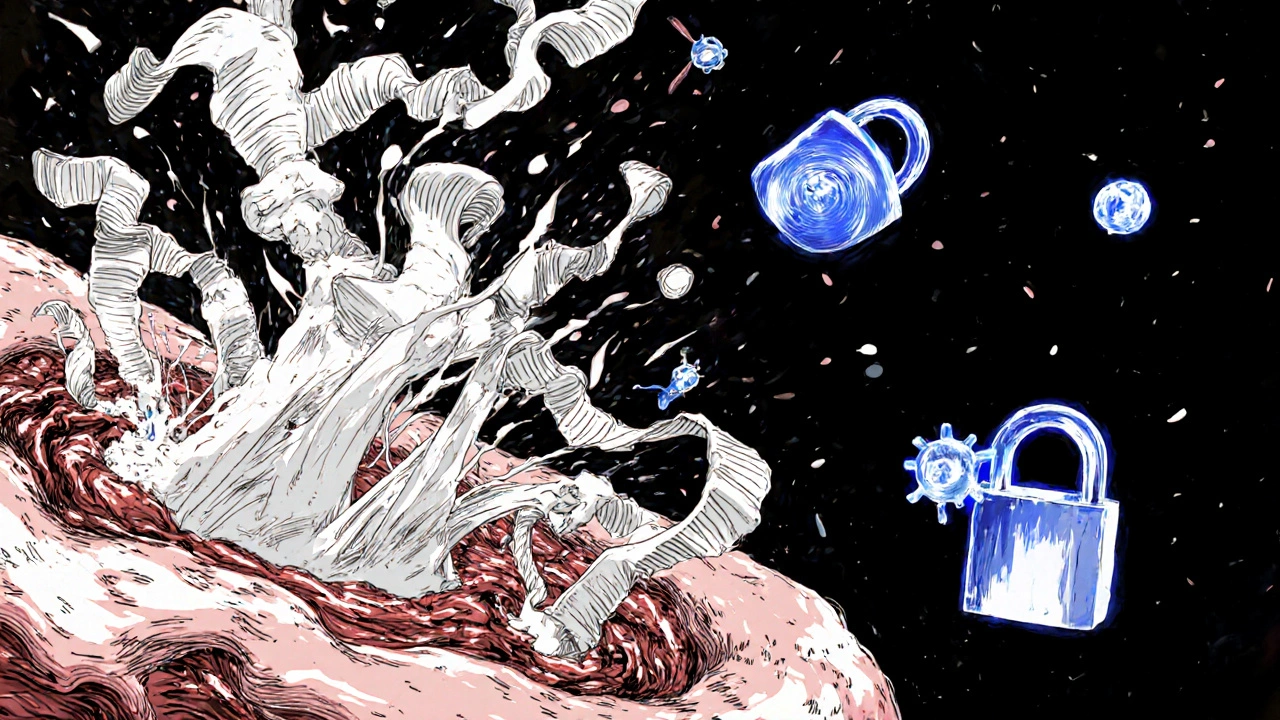
When you bleed, your body sends fibrin strands to form a mesh over the wound. That mesh holds platelets together to create a stable clot. But your body also releases enzymes-plasmin-that break down that mesh. It’s a natural cleanup system. In trauma, though, this cleanup goes haywire. Too much plasmin, too fast. Clots dissolve before they can do their job. That’s when tranexamic acid steps in.
It blocks plasmin from breaking down fibrin. Think of it like putting a lock on the demolition crew’s tools. The clot stays intact. Blood loss slows. The patient buys time.
This isn’t theory. In 2010, the CRASH-2 trial studied over 20,000 trauma patients across 27 countries. Those given tranexamic acid within three hours of injury had a 15% lower risk of dying from bleeding. No other drug had shown that kind of result in trauma care in decades.
Why timing is everything
Tranexamic acid isn’t magic. Give it too late, and it doesn’t work. Give it too early, and you risk clots forming where they shouldn’t-like in the brain or lungs.
The sweet spot? Within the first hour. After three hours, the benefit drops sharply. After four, it’s basically gone.
That’s why paramedics in places like London, Sydney, and Toronto now carry tranexamic acid in their ambulances. In rural Australia, where response times can stretch beyond 45 minutes, medics give it on scene. In emergency rooms, nurses prep the IV as soon as the patient rolls in. No waiting for lab results. No waiting for a doctor’s order. If trauma is suspected and bleeding is likely, tranexamic acid goes in.
It’s cheap. A single dose costs less than $10. It’s stable at room temperature. No refrigeration needed. That’s why it’s now part of WHO’s Essential Medicines List. It’s one of the few trauma drugs that works equally well in a city hospital and a field clinic in a war zone.
Who benefits the most
Not everyone with a cut needs tranexamic acid. It’s not for minor scrapes or nosebleeds. It’s for major trauma-especially when there’s internal bleeding.
Studies show the biggest gains come from:
- Patients with penetrating injuries (gunshots, stabbings)
- Those with blunt trauma from car crashes or falls
- People showing signs of shock-low blood pressure, fast heart rate, pale skin
- Women with postpartum hemorrhage (a separate but related use)
It’s less effective in patients with mild bleeding or those who’ve already lost over 40% of their blood volume. At that point, you need blood transfusions, surgery, and other interventions. Tranexamic acid doesn’t replace those. It just makes them more likely to work.
One study from the Royal Adelaide Hospital tracked 800 trauma patients over two years. Those who got tranexamic acid within 60 minutes were 2.3 times more likely to survive without needing a massive transfusion. That’s not a small number. That’s life or death.
Myths and misconceptions
Some doctors still worry it causes blood clots. That fear comes from older studies on people with stroke or heart disease-groups where tranexamic acid isn’t used. In trauma patients, the risk of dangerous clots is no higher than in those who didn’t get it.
A 2023 meta-analysis of 31 trials involving over 45,000 trauma patients found no increase in heart attacks, strokes, or pulmonary embolisms linked to tranexamic acid. The body doesn’t suddenly turn into a clotting machine. It just stops breaking down the clots it already made.
Another myth: it’s only for hospitals. That’s outdated. In Australia, the Royal Flying Doctor Service now carries it on every flight. In rural clinics, it’s stocked alongside epinephrine and IV fluids. In the U.S., the Army started giving it to soldiers on the battlefield in 2012. Survival rates jumped.
It’s not a cure-all. But it’s one of the few tools in emergency medicine that actually changes outcomes.

How it’s changing trauma care
Before tranexamic acid, trauma care was reactive. You gave fluids to keep blood pressure up. You packed wounds. You rushed to surgery. But if the patient bled out before getting to the OR, nothing helped.
Now, it’s proactive. You treat the bleeding at the same time you treat the injury. It’s part of the ‘Stop the Bleed’ philosophy now taught to first responders worldwide.
Hospitals have protocols. One dose: 1 gram IV over 10 minutes, followed by 1 gram over 8 hours. Some places give it as a single 3-gram dose. The key is speed, not precision.
Even in places with limited resources, the impact is clear. In a 2024 study in rural Kenya, trauma centers that started using tranexamic acid saw a 30% drop in preventable deaths from bleeding. No new machines. No fancy labs. Just a simple pill dissolved in water and injected.
What’s next
Researchers are now testing tranexamic acid for other types of bleeding-brain injuries, gastrointestinal bleeds, even nosebleeds in people on blood thinners. Early results are promising.
There’s also work on oral forms. Imagine a trauma patient swallowing a tablet at the scene instead of waiting for an IV. That could be a game-changer for mass casualty events or remote disasters.
It’s not about replacing surgery or blood transfusions. It’s about making them work better. Tranexamic acid doesn’t fix the wound. But it gives the body time to heal it.
For the first time in modern medicine, we have a drug that doesn’t just treat symptoms. It interrupts the process that kills. And it’s cheap, safe, and simple enough to use anywhere.
That’s why tranexamic acid is now considered one of the most important advances in trauma care since the invention of the tourniquet.
Can tranexamic acid be used for minor cuts or nosebleeds?
No. Tranexamic acid is not recommended for minor bleeding like small cuts or occasional nosebleeds. It’s designed for severe, life-threatening hemorrhage-especially from trauma, surgery, or postpartum bleeding. Using it for minor cases offers no benefit and could expose patients to unnecessary risk, even if the risk is low.
How quickly does tranexamic acid work?
Tranexamic acid starts working within minutes after an IV dose. It doesn’t stop bleeding instantly, but it prevents clots from breaking down. This means blood loss slows over the next 30 to 60 minutes. The sooner it’s given after injury, the more effective it is-ideally within the first hour.
Is tranexamic acid safe for everyone?
For trauma patients, yes-when used correctly. Studies show no increase in heart attacks, strokes, or dangerous clots in this group. But it’s not safe for people with a history of blood clots in the legs or lungs, or those with active thrombosis. It’s also avoided in patients with severe kidney disease because it’s cleared by the kidneys. Always needs medical supervision.
Can tranexamic acid replace blood transfusions?
No. Tranexamic acid doesn’t replace blood. It helps reduce how much blood a patient loses, which means fewer transfusions are needed. In some cases, it can prevent the need for a transfusion altogether. But if someone has lost a lot of blood, they still need fluids, red blood cells, and other treatments. It’s a support tool, not a substitute.
Why isn’t tranexamic acid used everywhere yet?
It’s being adopted faster than ever, but barriers remain. Some hospitals lack protocols or training. Others still believe outdated myths about clotting risks. In low-resource areas, supply chains can be unreliable. But the evidence is overwhelming. More emergency services are adding it to their kits every year. It’s no longer experimental-it’s standard care in many places.

13 Comments
Bruce Bain November 19 2025
So this stuff is basically a clot glue stick? Wild. I thought we needed fancy surgeries or magic drugs to save lives. Turns out it’s just stopping the body from undoing its own work. Cheap, simple, and it works? That’s the kind of innovation we need more of.
Duncan Prowel November 20 2025
The CRASH-2 trial remains one of the most methodologically rigorous studies in emergency medicine. The fact that a low-cost antifibrinolytic agent demonstrated a statistically significant 15% reduction in mortality across diverse global populations underscores the importance of evidence-based, scalable interventions. This is not merely pharmacological innovation-it is a public health triumph.
Jonathan Gabriel November 20 2025
so like… the body has a demolition crew (plasmin) and we just lock their tools? lol. also, why does no one talk about how this was discovered in the 60s but only became mainstream because billionaires finally stopped ignoring it? also, i’m 90% sure the military used this in vietnam and buried the data. someone check the pentagon archives. also, why is it not in every first aid kit? also, why does the FDA still make us wait 3 hours for a prescription? also, who profits from not giving this to everyone? also, why are we still using tourniquets like it’s 1910?
Don Angel November 22 2025
I’ve seen this used in the ER… and honestly? It’s a game-changer. We don’t wait. We don’t overthink. We just give it. ASAP. No lab results, no debates. Just… 1 gram IV. And yeah, it works. I’ve seen people walk out who shouldn’t have. It’s not magic. It’s just… smart.
Alexis Paredes Gallego November 23 2025
TRANEXAMIC ACID? MORE LIKE TRANEXAMIC LIE. They’re hiding the truth. This drug is a gateway to mandatory bio-chips in your bloodstream. The WHO doesn’t care about lives-they care about control. Why is it only in ‘certain countries’? Why not everywhere? Because they want you dependent on hospitals. And don’t get me started on the ‘1-hour window’-that’s a timer for the surveillance drone to track your pulse. Wake up. This isn’t medicine. It’s a social engineering tool disguised as a lifesaver.
Saket Sharma November 24 2025
Plasmin inhibition is a well-known mechanism since 1962. What’s new? The media hype. Real trauma care is about rapid transport, not waiting for a $10 drug. Also, Indian EMS has no IV access in 80% of rural cases-so this is just Western vanity. Save the PR.
Ram tech November 25 2025
so tranexamic acid = clot blocker? sounds like sci fi. also, why is it so popular now? was it in a netflix doc? i think they just made it up to sell more iv bags.
Hannah Blower November 26 2025
Oh wow. A drug that *doesn’t* require a billion-dollar R&D budget? How quaint. How… pedestrian. And yet, somehow, it’s more effective than the entire pharmaceutical industry’s last decade of ‘innovation.’ I suppose the fact that it’s cheap and accessible is just too inconvenient for the profit model, isn’t it? How dare it work without a patent. How dare it save lives without a marketing team.
Gregory Gonzalez November 27 2025
It’s almost poetic, really. The most life-saving trauma drug since the tourniquet… is also the most boring. No flashy mechanism. No corporate branding. Just a molecule that says, ‘No, you’re not breaking that clot.’ How utterly… un-American. Where’s the app? The subscription model? The NFT co-pay?
Ronald Stenger November 27 2025
So now we’re giving foreign-made pills to American soldiers? Who approved this? I bet it’s made in China. Or India. Or someplace that doesn’t even have running water. Meanwhile, our own pharma companies are developing $500,000 gene therapies that don’t work half the time. This isn’t progress-it’s surrender.
Samkelo Bodwana November 28 2025
Let me tell you something from the Cape Flats: we don’t have ambulances that arrive in 10 minutes. We don’t have IVs on every street corner. But we do have trained community responders who carry tranexamic acid in their backpacks, right next to the clean bandages and bottled water. I’ve seen a 16-year-old boy survive a stabbing because someone gave him this drug before the police even arrived. It’s not about the cost. It’s about dignity. It’s about saying, ‘You matter, even if you’re poor, even if you’re in a township, even if the system forgot you.’ This drug doesn’t just stop bleeding-it restores hope.
Emily Entwistle November 29 2025
OMG this is so cool!!! 🤩 I had no idea something so simple could save lives like this!! 💖 I’m telling all my friends!! Also, I just donated to a trauma fund in Kenya!! 🙌 #TranexamicMagic #SaveLives #MedicineIsBeautiful
deepak kumar December 1 2025
Tranexamic acid is not new. We used it in rural India for postpartum hemorrhage since 2008 under WHO guidelines. The real story is not the drug-it’s the delay in global adoption. Hospitals in Delhi saved 40% more mothers with this before American ERs even heard the name. It’s not about technology. It’s about will. We had the science. The West just needed a peer-reviewed paper to believe it.