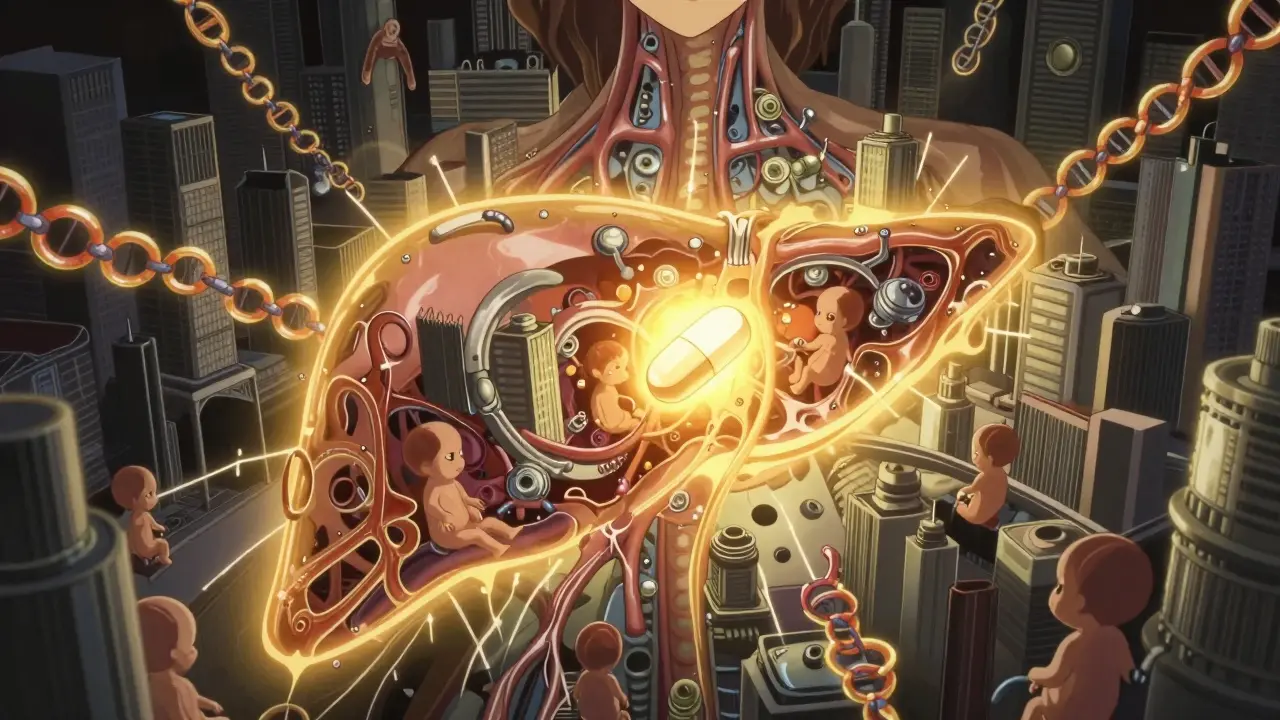
What Is Intrahepatic Cholestasis of Pregnancy?
Imagine your body’s natural detox system-bile-getting stuck. That’s essentially what happens in intrahepatic cholestasis of pregnancy (ICP), also known as obstetric cholestasis. It’s a liver condition that only occurs during pregnancy, and it’s not caused by anything you did. Hormones, especially estrogen, interfere with how bile flows out of your liver. Instead of moving normally into your intestines to help digest food, bile acids build up in your blood. This triggers one main symptom: intense itching, usually on your palms and soles, that gets worse at night. There’s no rash, no redness-just an overwhelming, unrelenting itch that doesn’t respond to lotions or antihistamines.
ICP shows up mostly in the late second or early third trimester, when hormone levels peak. In most cases, it disappears within a few days after delivery. But while it’s not dangerous for you in the long term, it carries serious risks for your baby. Studies show that when bile acid levels climb above 100 µmol/L, the risk of stillbirth jumps to 3.4%, compared to just 0.28% when levels stay below that. That’s why early detection and careful monitoring aren’t optional-they’re lifesaving.
How Do You Know If You Have It?
The biggest red flag is severe itching without a rash. If you’re scratching constantly, especially at night, and nothing helps, talk to your provider. But itching alone isn’t enough for a diagnosis. The gold standard test is a blood test for serum bile acids. Levels above 10 µmol/L confirm ICP. If they’re above 40 µmol/L, it’s considered severe. Above 100 µmol/L? That’s a major warning sign.
Doctors also check liver enzymes like ALT and AST. In about 60-70% of cases, these are elevated, but they can be normal even when bile acids are high. That’s why relying on liver tests alone can miss ICP. A newer marker called autotaxin is showing promise-studies found it’s 98.6% accurate at identifying ICP, but it’s not widely available yet. The key takeaway? If you have unexplained itching in late pregnancy, ask for a bile acid test. Don’t wait for your provider to bring it up. Only 42% of OB-GYN practices in the U.S. screen routinely unless symptoms are obvious, and delays in diagnosis average 7 to 10 days.
Who’s at Risk?
ICP doesn’t happen randomly. Certain factors make it much more likely. If you’re carrying twins or triplets, your risk triples or even quadruples. Women who got pregnant through IVF are twice as likely to develop it. And if your mom or sister had ICP, your risk is 12 to 15 times higher. Genetics play a big role here.
Geography matters too. In the U.S., about 1 to 2 out of every 1,000 pregnancies are affected. But in Chile, it’s as high as 15.6%. Latina women in general have a 5.6% rate. In the UK, it’s closer to 0.7-1.5%. These differences point to genetic and environmental factors still being studied. If you’re from a high-risk population or have a family history, make sure your provider knows. Early screening could make all the difference.

Why Is It Dangerous for the Baby?
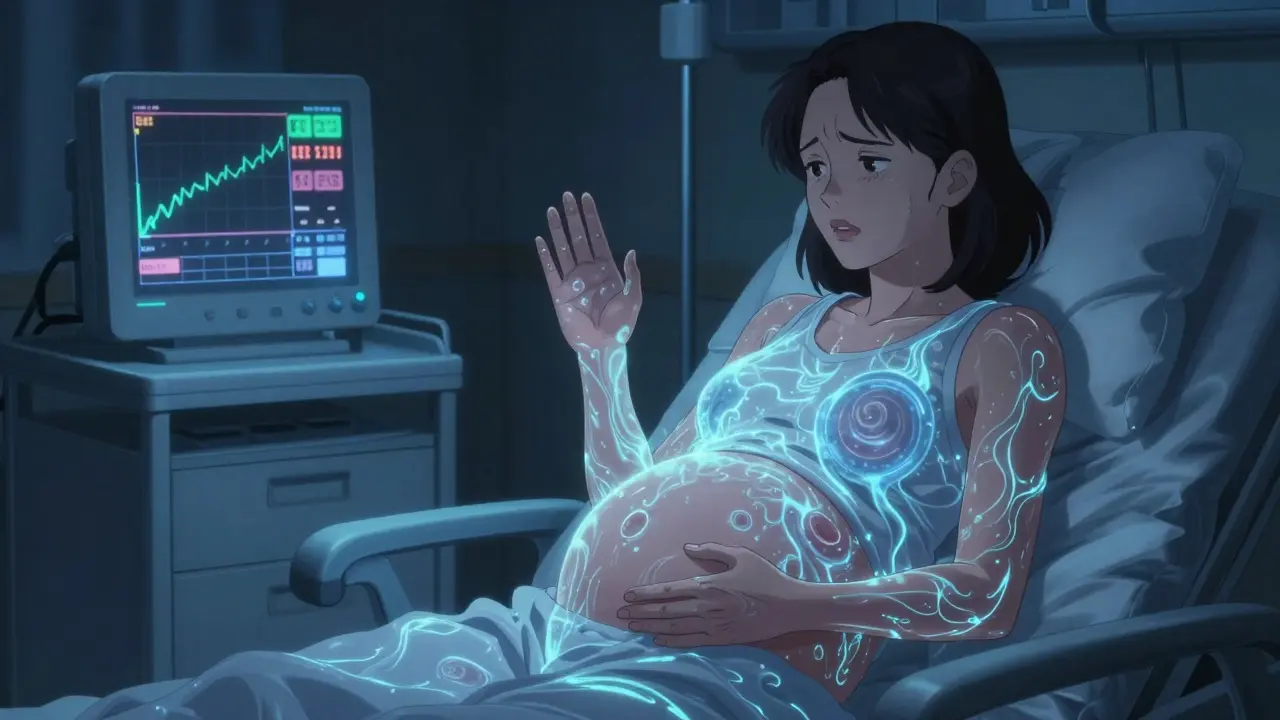
ICP doesn’t hurt you the way it hurts your baby. The high bile acid levels in your blood can stress the fetus. That’s why the biggest concern is stillbirth-especially when levels are high and not monitored. The risk rises sharply above 40 µmol/L, and even more so above 100 µmol/L. Preterm labor happens in 30-60% of ICP cases, depending on how high the bile acids climb and when you’re diagnosed. Some babies also experience fetal distress during labor, which can lead to emergency C-sections.
That’s why close monitoring is non-negotiable. The American College of Obstetricians and Gynecologists recommends twice-weekly non-stress tests starting at 32 to 34 weeks. These tests check your baby’s heart rate in response to movement. If everything looks good, your provider may recommend delivery between 37 and 38 weeks for mild cases. For severe cases-bile acids over 100 µmol/L-delivery might be suggested as early as 34 to 36 weeks. The goal isn’t to deliver too early, but to deliver before the risk spikes.
What Treatments Are Safe During Pregnancy?
The first-line treatment is ursodeoxycholic acid (UDCA). It’s taken as a pill, usually 10 to 15 mg per kilogram of your body weight per day. Studies show it reduces itching by about 70% and may lower the chance of preterm birth by 25%. It’s been used safely for decades in pregnancy, with no proven harm to the baby. Even though a 2022 Cochrane Review says there’s not enough evidence to prove it reduces stillbirth, most specialists still use it because it improves symptoms and quality of life-and there’s no better option.
If UDCA doesn’t work or causes side effects like diarrhea, there are alternatives. S-adenosyl methionine (SAMe) is sometimes used. Small studies show it cuts itching by 40-50%, but the evidence is limited. Cholestyramine is another option, but it’s not ideal. It can interfere with vitamin K absorption, which increases the risk of postpartum bleeding. It also causes bloating and constipation, which are already common in pregnancy.
There’s no magic cure, but treatment isn’t just about feeling better. It’s about reducing risk. UDCA lowers bile acid levels, and lower levels mean a safer pregnancy for your baby.
What’s New in ICP Care?
Things are changing fast. In 2023, the FDA approved a new point-of-care test called CholCheck®. It gives bile acid results in 15 minutes instead of waiting 1 to 3 days for lab results. That means faster diagnosis and quicker treatment decisions. It’s already in use in 65% of high-risk maternity hospitals in the U.S.
Research is moving toward personalized care. Instead of just checking bile acids once, doctors are tracking how they change over time. One study found that 30% of women go from mild to severe ICP in just two weeks. That’s why repeat testing every 1 to 2 weeks is now standard. The upcoming 2024 International Cholestasis of Pregnancy Consensus Statement is expected to recommend delivery at 38 weeks for mild cases if bile acids are stable and closely monitored-instead of pushing for earlier delivery. This could prevent unnecessary preterm births while keeping babies safe.
On the horizon are new drugs targeting autotaxin, an enzyme linked to itching in ICP. Phase II trials show a 68% reduction in itch severity after four weeks. These could be game-changers, but they’re still years away from being available.
What About Long-Term Health?
Even after delivery, ICP doesn’t just vanish without consequences. Women who’ve had it are 3.2 times more likely to develop liver or gallbladder problems later in life. That includes gallstones (4.3 times higher risk), chronic hepatitis (3.1 times higher), and even hepatitis C (2.8 times higher). It’s not guaranteed-you won’t definitely get these conditions-but your risk is significantly elevated. That means you should tell any future doctor about your ICP history. Regular liver checks and avoiding alcohol or unnecessary medications can help protect you.
What Should You Do If You’re Diagnosed?
First, don’t panic. ICP is manageable with the right care. Find a maternal-fetal medicine specialist. About 85% of major U.S. hospitals have standardized protocols, so ask if your provider follows them. Get your bile acids tested regularly. Stick with UDCA if it’s prescribed. Keep track of your baby’s movements-any sudden drop in activity means call your provider right away.
Education helps. Women who get detailed information about ICP report 22% lower anxiety and 18% better adherence to treatment. Ask for printed materials or trusted websites. Know the signs of fetal distress: decreased movement, unusual cramping, or bleeding. And remember-this isn’t your fault. It’s a biological twist of pregnancy, not something you caused.
Where Is Care Still Falling Short?
Not everyone has access to the same level of care. In Scandinavia, all pregnant women get routine bile acid screening in the third trimester. Since 2018, Sweden has seen a 35% drop in ICP-related stillbirths. In the U.S., many women aren’t tested until they’re already suffering. In low-resource settings, doctors have to guess based on symptoms alone. One expert warns this could increase adverse outcomes by 40% compared to places with regular monitoring.
If you’re in a place where testing isn’t routine, be your own advocate. If you have severe itching, insist on a bile acid test. Push for a referral to a specialist. Your awareness could be the difference between a routine pregnancy and a preventable tragedy.
11 Comments
Iona Jane January 15 2026
This is all a lie. The FDA doesn't approve anything for pregnant women. They're just hiding the truth about glyphosate in your coffee and the 5G towers frying your liver. I had itching. No test. Just vanished after I stopped eating gluten and prayed to the moon. They don't want you to know.
Jaspreet Kaur Chana January 17 2026
Bro I remember my sister going through this in Mumbai, she was screaming at night like a banshee, no rash, just pure agony, and the doctors there were like 'oh it's normal' until her bile acids hit 120 and they rushed her to delivery at 34 weeks. Thank god she had a cousin who studied in the UK and told her to demand the test. In India, we don't even have the word 'cholestasis' in most regional languages, people think it's stress or bad food. This post is a godsend. If you're pregnant and itching like your skin is on fire, don't wait. Fight for that blood test. Your baby's life is not a suggestion.
Tom Doan January 17 2026
Fascinating. The fact that a condition with such a clear biomarker-bile acids above 10 µmol/L-is still not routinely screened in 58% of U.S. OB-GYN practices suggests either systemic negligence or a deliberate suppression of data. The 3.4% stillbirth rate at >100 µmol/L is statistically catastrophic, yet we treat this like a nuisance rather than a medical emergency. The Cochrane Review’s caution about UDCA’s impact on stillbirth seems less like scientific rigor and more like institutional cowardice. Why are we still debating treatment efficacy when the diagnostic threshold is unambiguous?
Sohan Jindal January 17 2026
This is why we can't have nice things. Feminist doctors pushing fake science. Bile acids? Please. It's just the baby moving. My wife had itching and they gave her pills and delivered early. Now the kid has anxiety. I bet this whole thing is funded by Big Pharma. They want you scared so you take their drugs. No test. No pills. Just trust God and stop being so weak.
Frank Geurts January 17 2026
The introduction of CholCheck® represents a paradigmatic shift in perinatal hepatology: a point-of-care diagnostic modality that reduces diagnostic latency from 72 hours to 15 minutes, thereby enabling timely pharmacological intervention and optimizing perinatal outcomes. The statistical correlation between elevated bile acid levels and fetal demise is not merely correlative-it is causally inferable, and thus, the standard of care must be elevated accordingly. I commend the authors for their meticulous synthesis of longitudinal data and their advocacy for protocol standardization across geographies.
Annie Choi January 18 2026
I had ICP with both kids. First time I was ignored for 10 days. Second time I walked into my OB’s office with printed research and said ‘test me now or I’m going to the MFM.’ They did. Bile acids at 87. UDCA. Twice-weekly NSTs. Delivered at 37. Baby fine. I don’t care if your provider thinks it’s ‘just itching.’ If you’re awake at 3 a.m. clawing at your palms, you’re not imagining it. This isn’t anxiety. This is biochemistry screaming at you. Advocate. Hard.
Arjun Seth January 19 2026
You people are so obsessed with tests and pills. Back in my village, we used neem leaves boiled in water, rubbed on the skin, and drank turmeric milk. No hospital. No drugs. Baby born healthy at 40 weeks. Why do you trust chemicals from America more than your own ancestors? This is not medicine. This is colonialism in a lab coat.
Mike Berrange January 19 2026
I appreciate the data, but you didn't mention the psychological toll. The constant fear. The guilt. The way your partner looks at you like you're a ticking time bomb. I had ICP. UDCA helped the itching, but not the panic. I cried every time my baby moved. That's not in the guidelines. That's not in the Cochrane review. But it's real. And nobody talks about it.
Amy Vickberg January 20 2026
I'm so glad someone finally wrote this clearly. I was diagnosed at 35 weeks with bile acids at 110. I was terrified. But the MFM team had a plan. UDCA, NSTs twice a week, delivery at 36.5 weeks. Baby was perfect. No NICU. No trauma. Just a healthy 7lb 2oz girl. If you're reading this and itching-don't wait. Don't feel silly. Don't let your doctor dismiss you. You know your body. Push. Please. It's worth it.
Ayush Pareek January 22 2026
As a dad whose wife went through this, I want to say: you’re not alone. I didn’t know what to do. I just held her hand at night when she couldn’t sleep. I learned the bile acid numbers. I printed the guidelines. I showed them to her doctor. You don’t need to be a scientist. You just need to care enough to ask. And if your partner is suffering, be her voice when she’s too tired to speak.
Nishant Garg January 24 2026
In India, we call it 'pichhli maas ke baad ka kharas'-the itch that comes after the third month. Grandmas say it's the baby growing too fast. Doctors say it's 'hormonal imbalance.' No one says 'cholestasis.' But I read this and thought-this is exactly what my cousin went through. She lost her baby at 36 weeks. No test. No warning. If this post saves one child in a village clinic where they don't even have a microscope, it's worth every word.