Imagine sleeping through the night only to wake up bruised, with your partner bleeding from a punch you don’t remember throwing. Or finding yourself on the floor after kicking out in your sleep, convinced you were fighting off an intruder. This isn’t a nightmare-it’s REM sleep behavior disorder (RBD), a serious sleep condition where your brain fails to paralyze your muscles during dreaming. The result? You act out violent, vivid dreams, often with real-world consequences.
What Exactly Is REM Sleep Behavior Disorder?
During normal REM sleep, your body goes into temporary paralysis. This protective mechanism stops you from physically acting out your dreams. In RBD, that paralysis vanishes. Your arms, legs, and even vocal cords become active. You might yell, punch, kick, jump out of bed, or grab at imaginary objects. These episodes usually happen in the second half of the night, when REM sleep is most intense.
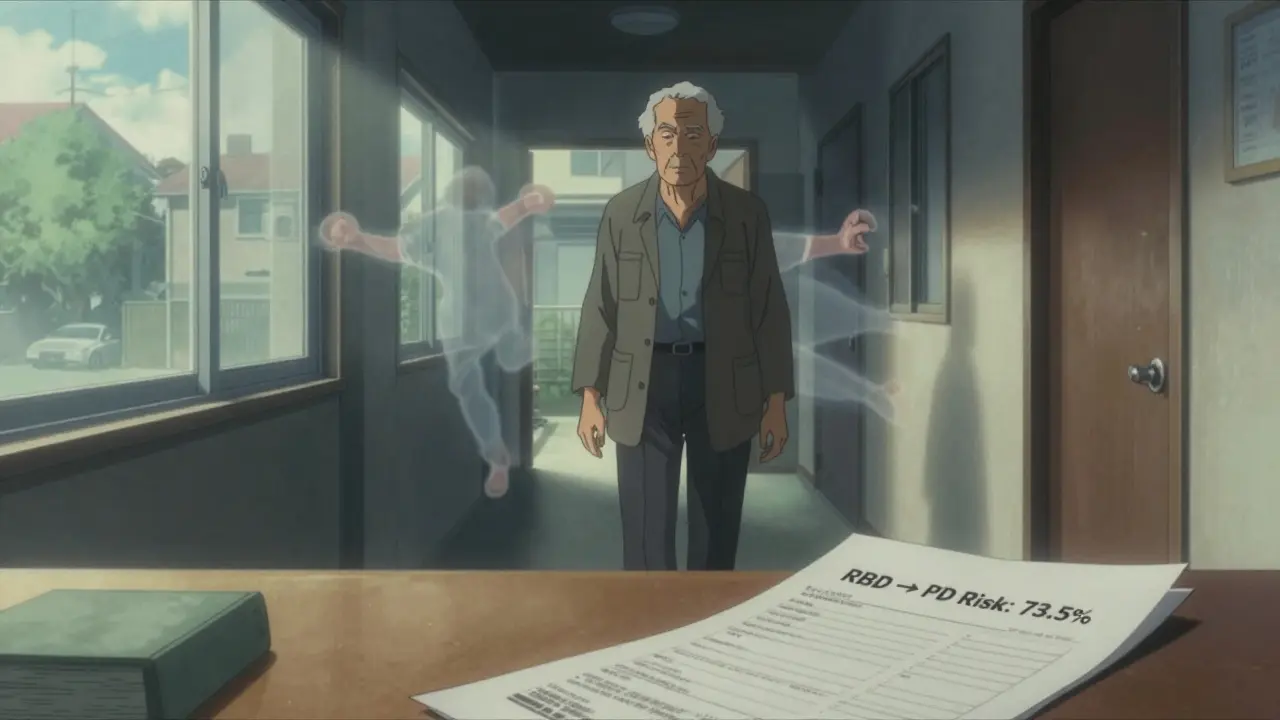
It’s not just a weird quirk. About 90% of people with RBD have an underlying neurological problem. Most commonly, it’s a synucleinopathy-conditions like Parkinson’s disease, dementia with Lewy bodies, or multiple system atrophy. Studies show that 73.5% of people with idiopathic RBD (meaning no known cause) will develop one of these disorders within 12 years. That makes RBD one of the strongest early warning signs we have for neurodegenerative disease.
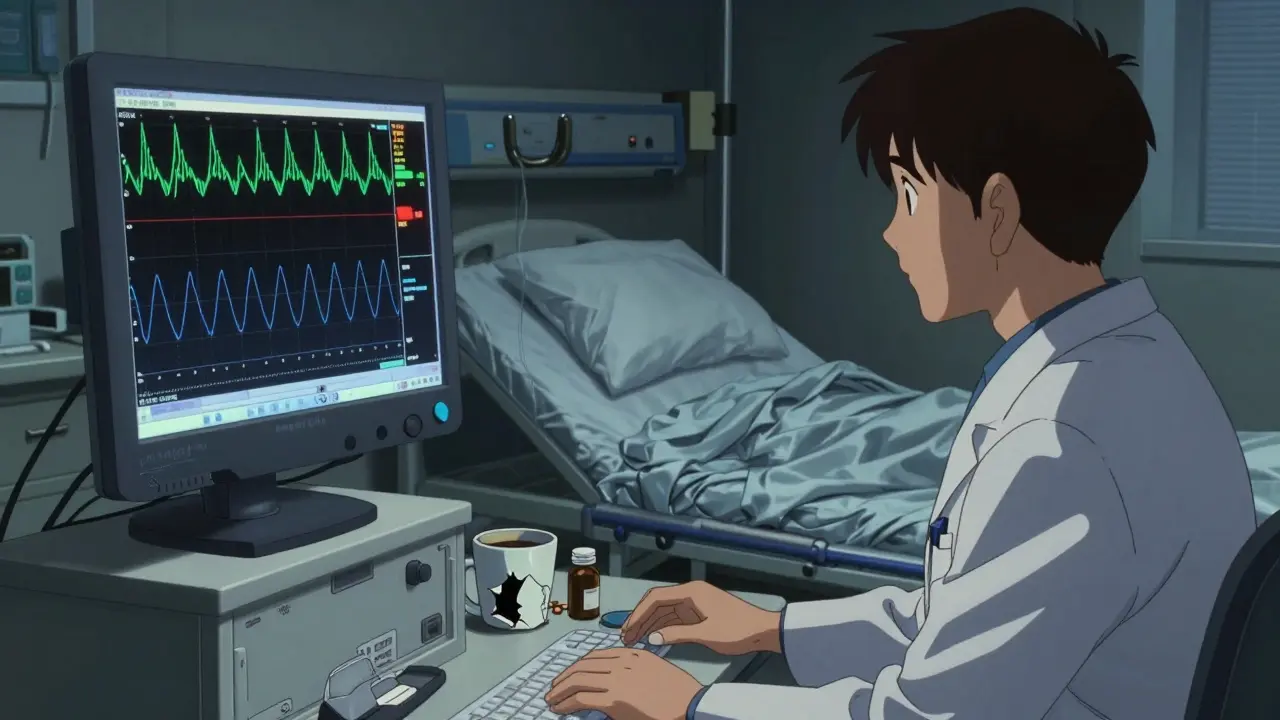
How Is RBD Diagnosed?
You can’t diagnose RBD with a questionnaire alone. The gold standard is a sleep study called polysomnography (PSG). During this overnight test, doctors monitor brain waves, eye movements, heart rate, breathing, and muscle activity. The key finding? REM sleep without atonia-meaning your muscles aren’t paralyzed when they should be.
The International Classification of Sleep Disorders, Third Edition (ICSD-3), requires that at least 15% of REM sleep epochs show abnormal muscle activity. In practice, patients often have complex movements happening 4.2 times per hour on average. That’s not occasional twitching-it’s frequent, dangerous behavior.
Doctors also look for a pattern: older men (over 50) with sudden onset of violent dream enactment, no history of seizures or psychiatric illness, and no recent use of antidepressants or alcohol. If this fits, RBD is likely.
First-Line Medications: Melatonin vs. Clonazepam
There are no FDA-approved drugs specifically for RBD. But two medications are widely used-and they work very differently.
Melatonin is a natural hormone your body makes to regulate sleep. In RBD, doctors prescribe it in much higher doses than you’d get over the counter. Typical starting dose: 3 mg at bedtime. Most patients increase gradually-6 mg, then 9 mg, up to 12 mg-waiting 2 to 4 weeks at each level to see if symptoms improve.
Why try melatonin first? It’s safe. In clinical studies, about 65% of patients see a major reduction in dream enactment. Side effects? Mild. Headache, dizziness, or morning grogginess in just 8% of users. One 68-year-old man went from 7 episodes a week to just 1 after starting 6 mg nightly. His only complaint? A little grogginess that faded after two weeks.
Clonazepam, a benzodiazepine, has been used for decades. It works by calming brain activity. Starting dose: 0.25-0.5 mg at bedtime. Maximum dose: 2 mg. It’s highly effective-80-90% of patients respond. A 2000 study found 88.7% symptom reduction. But it comes with serious risks.
Side effects include dizziness (22%), unsteadiness (18%), and daytime sleepiness (15%). In older adults, these increase fall risk by 34%. One patient stopped clonazepam after three months because falls went from zero to two per month. Long-term use can lead to dependence. Abruptly stopping it causes withdrawal nightmares in 38% of people. Tapering slowly-by 0.125 mg every 1-2 weeks-is essential.
Other Medications and Emerging Treatments
Some patients don’t respond to melatonin or clonazepam. Others can’t tolerate the side effects. That’s where alternatives come in.
Pramipexole, a dopamine agonist used for Parkinson’s and restless legs, helps about 60% of RBD patients. It’s often used when RBD overlaps with leg movements during sleep. Dose: 0.125-0.5 mg daily. But it’s not a first choice-it’s a backup.
Rivastigmine, a cholinesterase inhibitor, showed promise in a small trial for patients with RBD and mild cognitive impairment. It helped reduce episodes when other treatments failed. But it’s not widely recommended yet due to limited data.
The most exciting development? Dual orexin receptor antagonists. Orexin is a brain chemical that regulates wakefulness. Blocking it may calm overactive dreaming. Mount Sinai’s 2023 research found these drugs reduced dream enactment behaviors by 78% in animal models. Suvorexant (Belsomra), already approved for insomnia, is being tested for RBD. Neurocrine Biosciences’ NBI-1117568 received FDA Fast Track status in January 2023. If human trials succeed, this could be the first targeted RBD therapy with fewer side effects than clonazepam.
Neurological Monitoring: It’s Not Just About Sleep
Because RBD is often the first sign of Parkinson’s or dementia, neurological assessment is part of treatment-not an afterthought.
The American Academy of Neurology recommends annual check-ups for all idiopathic RBD patients. Why? The conversion rate to neurodegenerative disease is 6.3% per year. That means nearly one in 16 people with RBD will develop Parkinson’s or similar within a year.
Doctors look for subtle signs: slight tremors, reduced arm swing while walking, constipation, loss of smell, or mood changes. Early detection means earlier intervention. Drugs like levodopa or dopamine agonists can slow symptom progression if started early.
Some patients are enrolled in research studies tracking biomarkers-like alpha-synuclein levels in spinal fluid or brain imaging-to predict disease progression. These aren’t standard yet, but they’re the future.
Safety First: Changing Your Bedroom
Medication helps-but it doesn’t eliminate risk. You still need to make your bedroom safe.
The American Brain Foundation recommends:
- Remove all weapons, sharp objects, and glass from the bedroom
- Pad sharp corners of furniture
- Place thick rugs or mats beside the bed
- Install bed rails or sleep on a mattress on the floor
- Avoid alcohol-even one or two drinks can trigger episodes in 65% of people
78% of patients with RBD make these changes. Still, 42% end up sleeping separately from their partners, even with medication. One spouse said: “After my husband started 0.5 mg clonazepam, I could finally sleep in the same bed without fear of being kicked or punched.” That’s the goal-but safety comes first.
What’s Next for RBD Treatment?
The field is shifting. We’re no longer just treating symptoms. We’re trying to stop the disease before it starts.
With RBD as a predictor, researchers are testing drugs that target the underlying neurodegeneration-like alpha-synuclein antibodies or anti-inflammatory agents. Dr. Ronald Postuma from McGill University says: “The next five years will likely see the first disease-modifying therapies for RBD.”
Right now, we manage dreams. Soon, we may prevent Parkinson’s.
Final Thoughts
RBD isn’t just a sleep problem. It’s a neurological red flag. If you or someone you know is acting out dreams, don’t ignore it. See a sleep specialist. Get a sleep study. Start treatment. Make your home safe. And prepare for the long-term: neurological monitoring could save more than your sleep-it could delay or even prevent a life-altering disease.

11 Comments
Sarah B February 7 2026
This is why we need to stop treating sleep like it's optional. If you're punching your partner in the sleep you're not being lazy you're sick and someone needs to take that seriously. No more brushing it off as just bad dreams.
Tola Adedipe February 9 2026
I've seen this in my dad. He started kicking out in his sleep 5 years ago. We thought it was stress. Turned out it was early Lewy body dementia. This article nailed it. Melatonin helped but not enough. We had to pad the whole room. Scary stuff.
Eric Knobelspiesse February 10 2026
So let me get this straight. You're telling me that if I start sleep punching my wife I'm basically a walking Parkinson's warning label? Like my brain is just a ticking time bomb with REM dreams as the countdown? I mean yeah I dreamt I was fighting a dragon last night but also I'm 42 and I drink coffee at 9pm so... is this really neurodegeneration or just bad life choices lol
Marcus Jackson February 11 2026
Clonazepam works but the next day you feel like a zombie. Melatonin is safer but takes forever to kick in. I tried both. Went with 9mg melatonin. Took 6 weeks. Now I sleep like a baby. Still sleep on the floor though. Better safe than sorry.
Natasha Bhala February 13 2026
I'm so glad this got shared. My mom has RBD and we never knew what was happening. We thought she was having seizures. Sleep study changed everything. Now she's on melatonin and her arms don't look like she's been in a fight anymore. Small wins matter.
Jesse Lord February 13 2026
The safety tips here are gold. We removed all the glass and put a mattress on the floor. Best decision we ever made. My wife says she finally sleeps through the night. No more bruises. No more panic. Just peace. And yeah I know alcohol triggers it. I gave up my nightly whiskey. Worth it.
Catherine Wybourne February 15 2026
I'm British and I've never heard of this until now. We treat sleep disorders like they're just 'weird habits'. This is terrifyingly common. And the Parkinson's link? That's not a coincidence. It's a warning bell. We need public awareness. Not just for patients but for GPs too.
Amit Jain February 15 2026
LMAO people are losing their minds over dreaming they're fighting intruders? My cousin is a cop. He dreams he's shooting bad guys every night. Woke up with a broken lamp once. He just says 'that's Tuesday'. Stop medicalizing normal weird dreams. This is just anxiety in disguise.
Niel Amstrong Stein February 17 2026
Dual orexin antagonists?? 🤯 That's wild. Like literally hacking the dream engine. If this works we might be able to turn off nightmares on demand. Imagine not having to fear your own brain. 🤖💤 I'm all for it. Also Suvorexant sounds like a villain from a sci-fi movie.
Joey Gianvincenzi February 17 2026
It is imperative that medical professionals recognize REM sleep behavior disorder not as an isolated sleep anomaly but as a prodromal manifestation of alpha-synucleinopathies. The imperative for early neurological surveillance cannot be overstated. Furthermore, the pharmacological interventions outlined require rigorous clinical validation prior to widespread adoption.
Ritu Singh February 19 2026
In India, we call this 'jaadu ki nind'-magic sleep. No one takes it seriously. My uncle had this for 12 years. He broke his hip jumping out of bed. No one connected it to Parkinson's until it was too late. This needs to be talked about. In homes. In clinics. Everywhere.