When you start taking a statin to lower your cholesterol, the last thing you want to hear is that it might be hurting your liver. But if your blood test shows elevated liver enzymes, it’s natural to panic. You’re not alone. Many people stop their statins because of this - even though the real risk is tiny. The truth? Most of the time, those higher enzyme numbers don’t mean your liver is damaged. They’re just a signal - not a crisis.
What Do Elevated Liver Enzymes Actually Mean?
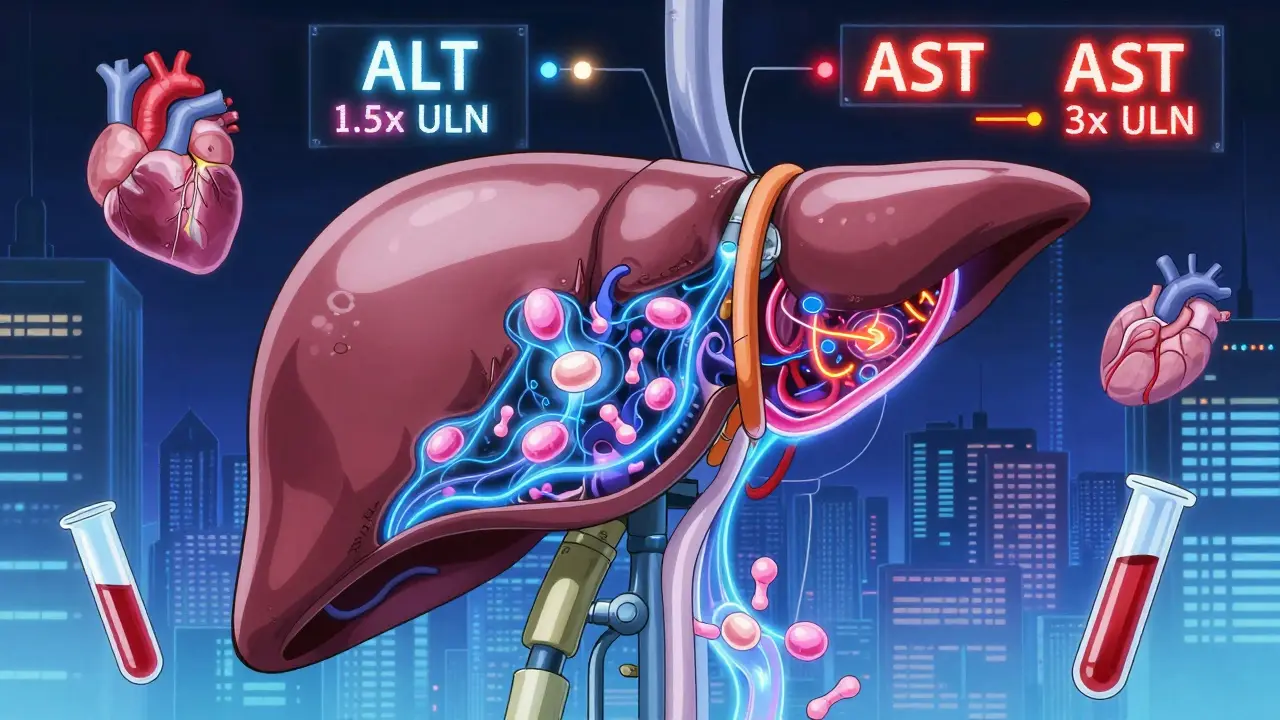
Liver enzymes like ALT (alanine aminotransferase) and AST (aspartate aminotransferase) are proteins found inside liver cells. When those cells get stressed or irritated, small amounts of these enzymes leak into the bloodstream. That’s what shows up on a blood test. But that doesn’t mean your liver is failing. It’s like a car’s check engine light - it’s telling you something’s off, but not necessarily that the engine is broken. Statin use can cause these enzymes to rise in about 0.5% to 2% of people. That’s less than 1 in 50. And in most cases, the numbers go back to normal on their own, even if you keep taking the statin. The FDA reviewed data from over 20 million patient-years and found only 32 confirmed cases of statin-induced liver failure since 1990. That’s 0.00016 cases per 1,000 people per year. You’re far more likely to be hit by lightning than to suffer serious liver damage from a statin.When Should You Worry?
Not all enzyme elevations are the same. The key number to watch is three times the upper limit of normal (3x ULN). If your ALT or AST is higher than that, your doctor may pause your statin temporarily. But if it’s below that - say, 1.5x or 2x ULN - you almost always should keep taking it. Studies show that continuing statins in these cases doesn’t increase the risk of liver harm. In fact, stopping them can be more dangerous. One study of veterans found that 18.7% of people stopped their statins just because their enzymes were mildly elevated. Within 18 months, 5 of those 17 patients had heart attacks or strokes. Their cholesterol was back up. Their arteries were getting worse. All because they misunderstood a lab result.Not All Statins Are the Same
Some statins are easier on the liver than others. Pravastatin and rosuvastatin are hydrophilic - meaning they don’t easily enter liver cells. That makes them less likely to cause enzyme spikes. Simvastatin and atorvastatin are lipophilic - they slip into liver cells more easily, which is why they’re more often linked to higher enzyme levels. Cerivastatin was the worst offender - it was pulled off the market in 2001 because of too many liver and muscle problems. But it’s no longer available. Today’s statins are much safer. In head-to-head trials, pravastatin caused elevated enzymes in only 0.3% of users. Atorvastatin? Around 1.2%. That’s still a very low risk.Who’s at Higher Risk?
Some people are more likely to see enzyme changes. If you’re over 75, have kidney disease (creatinine clearance under 30 mL/min), or are taking other drugs that affect liver metabolism, your risk goes up. Certain medications - like clarithromycin, itraconazole, or grapefruit juice - block the CYP3A4 enzyme, which helps break down some statins. That can cause statin levels to build up and stress the liver. There’s also a genetic factor. A variant in the SLCO1B1 gene makes it harder for your liver to clear statins. People with this variant have over three times the risk of enzyme elevations. A new genetic test called StatinSafety Plus can identify this, but it’s not routinely recommended unless you’re on high-dose statins or already have liver issues.
Don’t Blame the Statin - Check the Real Culprits
Before you assume your statin is the problem, rule out other causes. Nonalcoholic fatty liver disease (NAFLD) affects nearly half of adults with elevated liver enzymes. Alcohol use, viral hepatitis, and even certain supplements can raise ALT and AST. In fact, studies show that when doctors check for these other causes first, they reduce unnecessary statin stops by over 60%. Surprisingly, people with NAFLD actually have a lower risk of statin-induced enzyme spikes than those without it. The statins might even help their liver by reducing fat buildup. One study in Hepatology found NAFLD patients on statins had fewer enzyme elevations than healthy controls.What Should You Do If Your Enzymes Rise?
Here’s the practical guide:- Before starting: Get a baseline liver test. That’s all you need.
- After starting: No routine repeat tests unless you have symptoms - fatigue, nausea, dark urine, yellow skin, or belly pain.
- If enzymes are 1-3x ULN: Keep taking the statin. Retest in 4-6 weeks. Most will normalize.
- If enzymes are >3x ULN: Stop the statin temporarily. Recheck in 2-4 weeks. If levels drop, your doctor may restart you on a different statin - often pravastatin or fluvastatin.
- If symptoms appear: Stop immediately and call your doctor. This could be something else.
Why Do So Many People Stop Their Statins?
It’s not about the science. It’s about fear. A 2021 survey found that 68% of statin users were deeply worried about liver damage. But only 1.2% ever had enzyme levels above 3x ULN. That’s a huge gap between perception and reality. Doctors still order routine liver tests - even though the FDA, American College of Cardiology, and American Gastroenterological Association all say it’s unnecessary. In the U.S., that adds up to $1.27 billion a year in wasted testing. And it fuels anxiety. Patients see a slightly high number, panic, and quit. Then they end up with heart attacks because their cholesterol wasn’t controlled.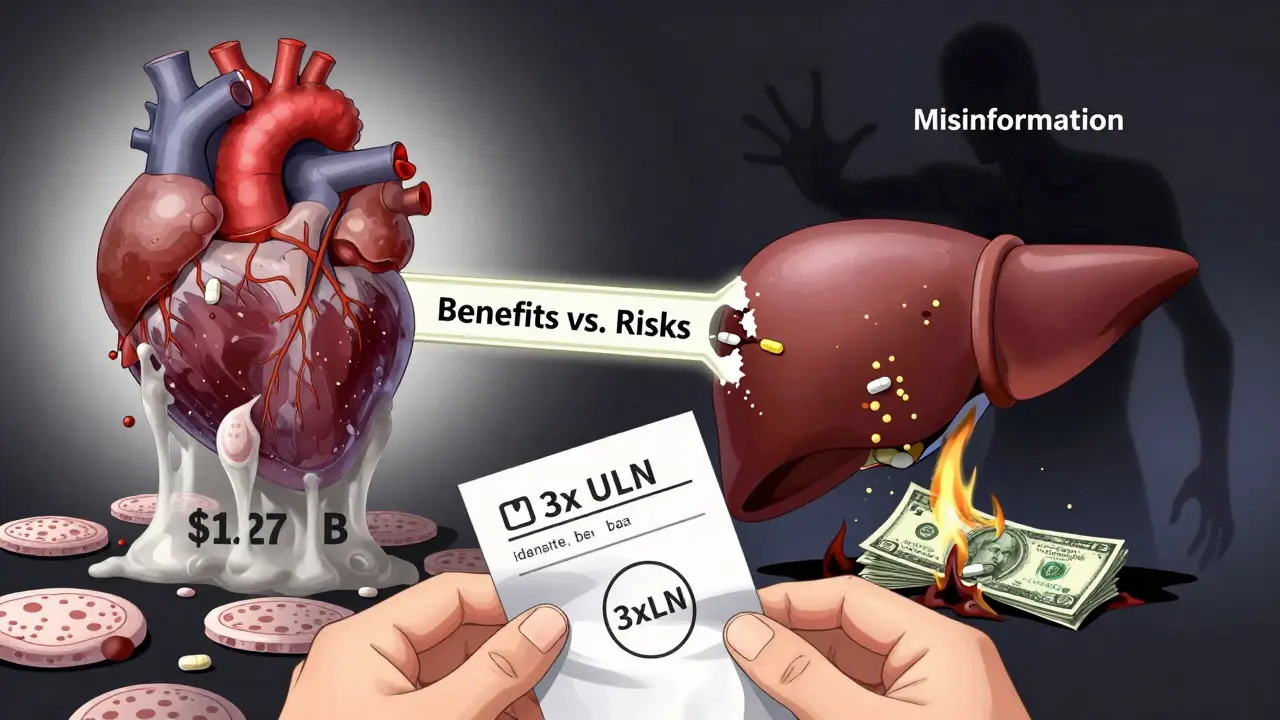
What About Supplements Like CoQ10?
Some people take CoQ10 to prevent statin side effects. There’s some evidence it helps with muscle aches. For liver enzymes, early trials show promise. One phase II study found CoQ10 reduced statin-related ALT elevations by 42.7%. But we don’t yet know if that translates to fewer heart attacks or strokes. It’s not a substitute for statins - just a possible helper.The Big Picture: Benefits vs. Risks
Statin therapy saves lives. For every 1,000 people treated with statins for five years, about 25 major cardiovascular events are prevented. That’s the number needed to treat. Now look at the liver risk: For every 1,000 people on statins, maybe one will have a significant enzyme rise - and even fewer will have real liver damage. The number needed to harm is over 1,000. The American Heart Association says it clearly: "The cardiovascular benefits of statins generally outweigh noncardiovascular harms including the hepatic adverse effects."Bottom Line: Don’t Quit Because of a Lab Number
Elevated liver enzymes on statins are common. Serious liver injury is not. If your numbers go up a little, don’t panic. Talk to your doctor. Get retested. Rule out other causes. Most likely, you’ll keep taking your statin - and keep your heart safe. If you’ve stopped your statin because of liver concerns, it’s not too late to restart. Many people do - after their doctor explains the numbers. And those who do? Their heart risk drops back down. Your liver is resilient. Your heart isn’t. Don’t trade one for the other.Do statins cause liver damage?
Serious liver damage from statins is extremely rare - less than 0.01% of users. Most cases involve mild, temporary rises in liver enzymes (ALT/AST), which often return to normal without stopping the medication. The FDA states that statins pose a very low risk of serious liver injury, and routine monitoring is no longer recommended.
What should I do if my liver enzymes are high on statins?
If your ALT or AST is less than three times the upper limit of normal and you have no symptoms, continue your statin and retest in 4-6 weeks. Most elevations resolve on their own. If levels exceed 3x ULN, your doctor may pause the statin, retest after 2-4 weeks, and then consider restarting a different statin like pravastatin or rosuvastatin.
Should I get regular liver tests while taking statins?
No. The FDA, American College of Cardiology, and American Gastroenterological Association all agree that routine liver function testing is unnecessary. Only test before starting the statin, and only retest if you develop symptoms like jaundice, nausea, or abdominal pain.
Are some statins safer for the liver than others?
Yes. Hydrophilic statins like pravastatin and rosuvastatin are less likely to cause liver enzyme elevations because they don’t penetrate liver cells as easily. Lipophilic statins like simvastatin and atorvastatin have slightly higher rates, but the overall risk remains very low for all.
Can I take statins if I have fatty liver disease?
Yes. In fact, people with nonalcoholic fatty liver disease (NAFLD) have a lower risk of statin-induced enzyme elevations than those without it. Statins may even help reduce liver fat and inflammation. Major guidelines now say NAFLD is not a reason to avoid statins.
Will CoQ10 protect my liver from statin damage?
CoQ10 may reduce statin-related liver enzyme elevations by about 43% in early studies, but there’s no proven long-term benefit for heart health. It’s not a replacement for statins, and it’s not routinely recommended - but it’s safe to try if you’re concerned. Always talk to your doctor first.
Why do doctors still order liver tests if they’re not needed?
Many doctors still follow old habits or respond to patient anxiety. Over 34% of primary care providers in the U.S. order routine liver tests despite clear guidelines against it. This costs over $1 billion a year and often leads to unnecessary statin discontinuation. The science is clear: routine testing doesn’t prevent harm - and can cause it.
8 Comments
Shane McGriff January 19 2026
I get it - you see a number go up on a lab report and your brain goes straight to ‘I’m dying.’ But seriously, statins aren’t the enemy here. My dad was on atorvastatin for 8 years, his ALT hovered at 1.8x ULN for years - no symptoms, no issues. He kept taking it. His cholesterol stayed under control. He’s still alive and biking every morning at 72. The real danger? Quitting because you panicked over a number that meant nothing.
pragya mishra January 20 2026
Ugh, another doctor pushing pills. You think liver enzymes are just ‘noise’? What about the people who get jaundice and end up in ICU? You’re downplaying real risks for profit. Pharma doesn’t care if you live or die - they just want you to keep buying.
sagar sanadi January 20 2026
LMAO so statins are fine? Sure. And the moon landing was real. You know what’s REALLY in those pills? That’s right - the government’s secret plan to make us all docile. Liver enzymes? Just a distraction so you don’t notice your kidneys are slowly turning to dust. Also, I heard they add fluoride to make you forget your own name. Just saying.
kumar kc January 21 2026
If you don’t listen to your doctor, you deserve a heart attack.
Renee Stringer January 22 2026
I just… I don’t know. I saw my ALT was 1.9x and I cried. I didn’t want to be one of those people who ignored the signs. Maybe I overreacted. But I’m scared. I don’t trust labs. I don’t trust doctors. I just want to be safe.
Thomas Varner January 23 2026
Okay, so… let me get this straight: the liver’s like a car’s check engine light, right? So if it’s on, you don’t turn off the car - you just… keep driving? And hope the light goes off? That’s wild. I mean, if my car’s light came on, I’d pull over and call a mechanic. Not just ‘eh, it’s fine.’ But hey, I guess if you’re already driving a 2008 Corolla with 200k miles… maybe you’re used to ignoring warnings. 🤷♂️
Emily Leigh January 24 2026
So… let me get this… you’re saying the entire medical system is just… gaslighting us? Like, they’re telling us to ignore a red flag because ‘the math says it’s fine’? But what if the math is wrong? What if the ‘0.00016%’ is just the tip of the iceberg and they’re hiding the rest? Also, I’m pretty sure I read somewhere that the FDA gets funding from pharma… so… yeah. I’m not restarting my statin. I’m going to juicing and turmeric. And maybe a crystal. For balance.
Jacob Cathro January 26 2026
Bro. Statins are just a 3000% markup on a molecule that’s been around since the 80s. They’re not ‘saving lives’ - they’re just keeping the pill mill running. And that ‘CoQ10 reduces ALT by 43%’ study? Phase II? That’s like saying ‘I tried this one guy’s TikTok cure and my acne cleared up.’ Also, who the hell still uses ‘ULN’? That’s not a word. It’s an acronym. Say ‘upper limit of normal.’ I’m not a lab tech. And also… why are we even talking about this? Just eat less bread. Problem solved. 💅