Corticosteroid Infection Risk Calculator
Your Corticosteroid Use
Your calculated infection risk:
Recommendations:
When you take corticosteroids like prednisone for conditions like rheumatoid arthritis, lupus, or severe asthma, you're getting powerful relief from inflammation. But there’s a hidden cost: your body’s ability to fight off infections drops significantly. This isn’t theoretical - it’s a real, measurable risk that affects thousands of people every year. The good news? You don’t have to accept it as inevitable. With the right strategies, you can stay protected without giving up the benefits of these drugs.
How Corticosteroids Weaken Your Immune System
Corticosteroids mimic cortisol, the body’s natural stress hormone. At normal levels, cortisol helps regulate immune responses. But when you take higher doses - like 20 mg or more of prednisone daily - you flood the system. This doesn’t just calm inflammation; it shuts down key parts of your defense system. The biggest damage is to T cells. These are the soldiers that hunt down viruses, fungi, and bacteria hiding inside your cells. Corticosteroids make T cells stop multiplying, reduce their movement through the body, and even trigger their death. Studies show this effect is similar to drugs like cyclosporine, but it works through different pathways. What’s worse? Your body’s macrophages - the cleanup crew that swallows up invaders - become sluggish. They stop presenting threats to other immune cells and lose their ability to stick to blood vessel walls and move into infected tissues. Interestingly, your B cells - responsible for making antibodies - aren’t hit as hard. That means you still produce antibodies, but without T cells doing their job, your body can’t respond effectively to intracellular threats like tuberculosis, Pneumocystis pneumonia, or shingles. This creates a dangerous blind spot: you might feel fine, but your defenses are quietly failing.Who’s at Highest Risk?
Not everyone on corticosteroids gets sick. Risk isn’t random - it’s predictable and tied to two things: dose and duration. If you’re taking 20 mg or more of prednisone daily for more than 3 to 4 weeks, your infection risk jumps sharply. Each additional 10 mg per day increases your chance of a serious infection by 32%, according to a major 2022 analysis. That means someone on 30 mg/day has nearly double the risk of someone on 10 mg/day. The most dangerous infections include:- Pneumocystis jirovecii pneumonia (PJP): Occurs in 1.5% to 5% of high-dose users. Mortality can hit 50% if not caught early.
- Tuberculosis reactivation: Risk increases up to 7.7 times in people on ≥15 mg/day for over a month, especially in areas where TB is common.
- Invasive fungal infections: Candida and Aspergillus can spread from the lungs to the brain or bloodstream.
- Herpes zoster (shingles): Incidence rises from 1.2-2.0 per 100 person-years in healthy people to 2.8-6.5 in steroid users.
Proven Ways to Prevent Infections
Prevention isn’t guesswork. There are clear, evidence-backed steps that work. 1. PJP Prophylaxis If you’re on ≥20 mg/day prednisone for more than 4 weeks, you need to take trimethoprim-sulfamethoxazole (Bactrim or Septra). This simple antibiotic reduces PJP risk from over 5% down to less than 0.3%. It’s taken once or twice a week and is usually well tolerated. Skip this, and you’re playing Russian roulette with your lungs. 2. TB Screening Before starting high-dose steroids (≥15 mg/day for >1 month), get tested for latent tuberculosis. Use either an interferon-gamma release assay (IGRA) or a tuberculin skin test. If it’s positive, treat it with a 3- to 4-month course of isoniazid or rifampin. This cuts reactivation risk by 90%. The WHO and CDC both insist on this step - yet many clinics still skip it. 3. Vaccinations - Timing Matters You need your flu shot, pneumococcal vaccine, and COVID-19 booster. But get them at least 2 weeks before starting steroids. Once you’re on high doses, your body’s antibody response drops. One 2023 study found only 42% of patients on >20 mg/day prednisone responded to the flu vaccine - compared to 78% in healthy people. Live vaccines (like MMR or shingles vaccine) are off-limits entirely while you’re immunosuppressed. 4. Monitor Your Blood A simple blood test can tell you if your immune system is in trouble. Check your absolute lymphocyte count (ALC). If it falls below 1,000 cells/μL, you’re in high-risk territory. Monthly CBCs during long-term therapy help catch problems before they become infections.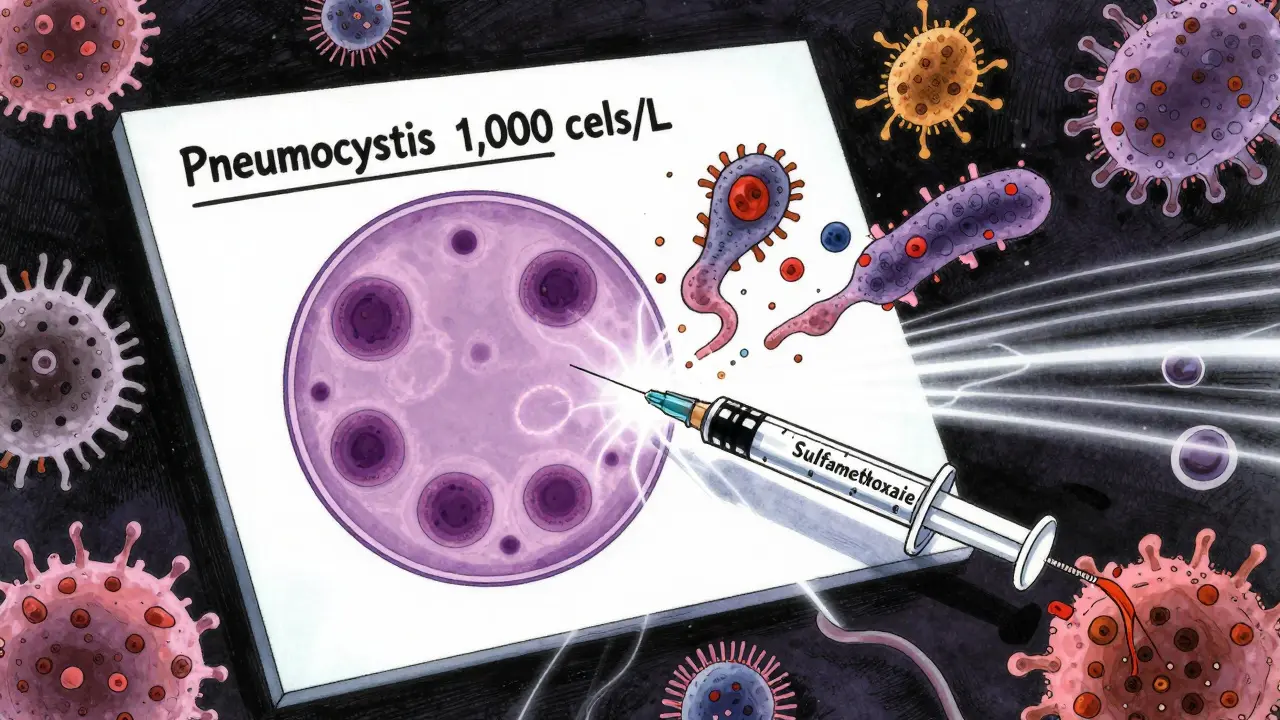
Lower the Dose - It’s the Best Strategy
The single most effective way to reduce infection risk? Use the lowest possible dose for the shortest time. Doctors are trained to start high and taper slowly. But research shows that rapid tapers - cutting doses faster than usual - reduce infection rates by 37%. A 2022 study in Arthritis & Rheumatology found patients who tapered aggressively had fewer infections, no increase in disease flares, and better long-term outcomes. That’s why experts now recommend adding steroid-sparing agents early. If you have autoimmune disease, start methotrexate, azathioprine, or a biologic within 4 weeks of beginning steroids. These drugs control inflammation so you can reduce or stop steroids sooner. One patient on Reddit put it plainly: “My rheumatologist switched me to methotrexate after 3 months on prednisone. I haven’t had a cold since.”What You Should Watch For
You can’t rely on classic signs of infection. No fever? Don’t assume you’re fine. Watch for:- New or worsening cough, shortness of breath, or chest pain
- Unexplained fatigue or night sweats
- Skin rashes, especially blisters or red patches (could be shingles)
- Diarrhea that doesn’t go away
- Swollen lymph nodes or persistent headaches
Where the System Falls Short
Real-world data from the FORWARD registry shows only 52% of patients on long-term steroids get proper infection prophylaxis. That’s not because doctors don’t know - it’s because systems are broken. Prescriptions don’t auto-populate. Patients aren’t always educated. And many don’t realize they’re at risk. A 2022 study found patients who received structured education about infection symptoms had 28% fewer hospitalizations. Simple things - like handing out a one-page handout on warning signs - make a huge difference.The Future: Smarter Steroids
Science is working on solutions. A new class of drugs called selective glucocorticoid receptor modulators (SEGRMs) is showing promise. Vamorolone, for example, works like prednisone to reduce inflammation but causes 47% fewer infections in clinical trials. It’s already approved for Duchenne muscular dystrophy. Researchers are also developing genomic tests to predict who’s most vulnerable to steroid-induced immunosuppression. Within five years, we may be tailoring prophylaxis based on your DNA - not just your dose. But for now, the tools we have are powerful. Use them.Can I take live vaccines while on corticosteroids?
No. Live vaccines - including MMR, varicella (chickenpox), and the older shingles vaccine (Zostavax) - are strictly off-limits while you’re on high-dose corticosteroids. These vaccines contain weakened viruses that your suppressed immune system can’t handle, which could cause serious infection. Wait until you’ve stopped steroids and your immune system recovers - usually 3 to 6 months after stopping. Inactivated vaccines (like flu shot, pneumococcal, or COVID-19 mRNA shots) are safe and recommended, but give them at least 2 weeks before starting steroids for best results.
Is there a safe dose of prednisone that doesn’t increase infection risk?
There’s no completely safe dose, but risk is very low below 5 mg/day of prednisone for most people. At this level, the immunosuppressive effect is minimal, especially if taken every other day. However, even low doses can pose risks if taken for years, particularly in older adults or those with diabetes or lung disease. The key is duration. A 5 mg/day dose for 6 months carries more risk than 20 mg/day for 2 weeks. Always aim for the lowest dose that controls your condition.
Why do I need to be screened for TB before taking steroids?
Corticosteroids can reactivate latent tuberculosis - meaning the bacteria that have been sleeping in your lungs for years can suddenly wake up and cause active, contagious disease. This happens because steroids suppress the T cells that keep TB under control. In some countries, up to 1 in 3 people carry latent TB. If you’re on ≥15 mg/day prednisone for over a month, your risk of reactivation increases 7-fold. Screening with a blood test (IGRA) or skin test lets doctors treat the hidden infection before it becomes dangerous.
Can I stop taking my prophylaxis if I feel fine?
No. Even if you feel healthy, stopping prophylaxis too soon leaves you vulnerable. Pneumocystis pneumonia often develops silently. You may not have symptoms until it’s advanced. Prophylaxis should continue for as long as you’re on ≥20 mg/day prednisone equivalent. Only stop after your doctor confirms you’ve tapered below that threshold and stayed there for at least 4 weeks. Never stop based on how you feel.
Do I need a chest X-ray if I’m on long-term steroids?
If you’re on ≥15 mg/day prednisone for more than 3 months - especially if you live in or traveled to a TB-endemic area - monthly chest X-rays are recommended. They catch early signs of TB or fungal pneumonia before symptoms appear. In places like Southeast Asia, Africa, or parts of Eastern Europe, this is non-negotiable. Even in low-risk areas like New Zealand or Canada, it’s still advised for patients on long-term high-dose therapy. Don’t wait for a cough to start screening.