When someone you love dies, it’s normal to feel broken. You cry. You can’t sleep. You lose interest in food, in friends, in life. But is this grief-or is it depression? The difference isn’t just academic. It determines whether you need a therapist who specializes in loss, or a doctor who prescribes medication. It decides if you heal by remembering your loved one-or by rebuilding your sense of self.
What Grief Really Feels Like
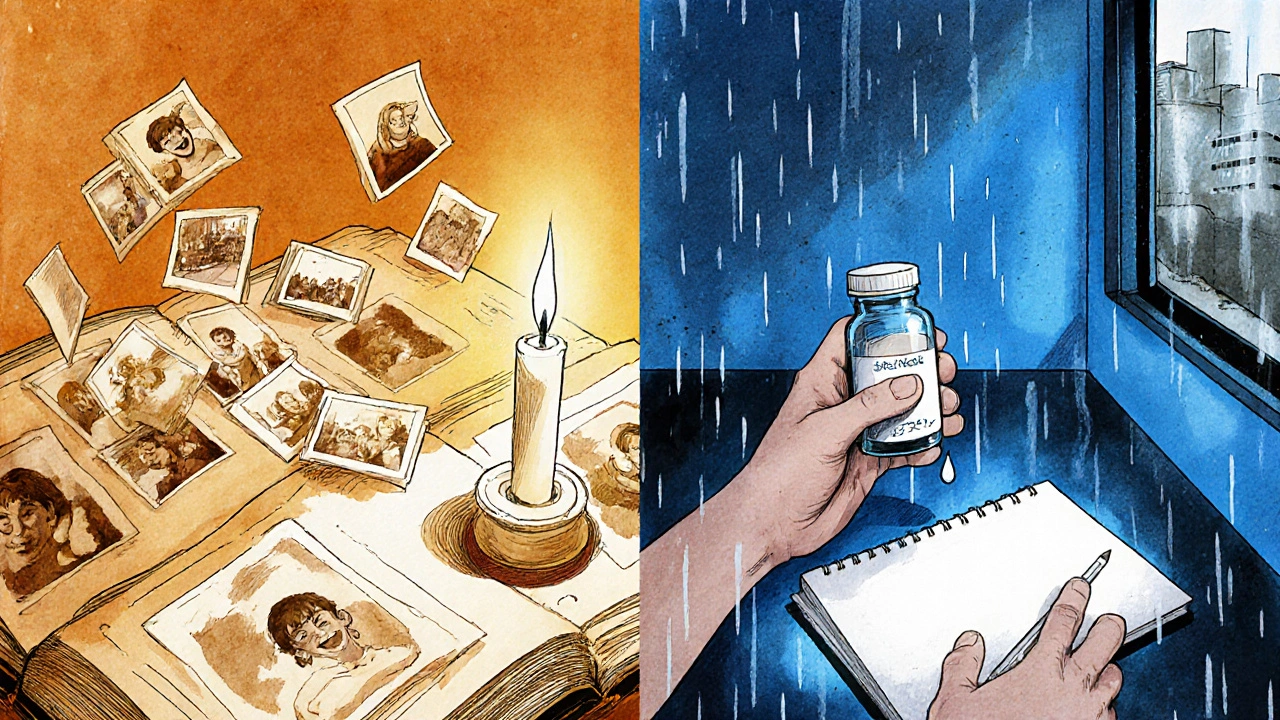
Grief isn’t a linear path. It doesn’t follow five neat stages like denial, anger, bargaining, depression, and acceptance. That model, from Elisabeth Kübler-Ross in 1969, made sense as a metaphor-but real grief is messier. It comes in waves.You’re making coffee one morning, and you smell their favorite blend. Suddenly, you’re laughing at a memory. Then, five minutes later, you’re on the floor, sobbing. That’s grief. It’s not constant sadness. It’s pain mixed with love. You feel the absence, but you also feel them-through photos, songs, habits, even their old jacket still hanging in the closet.
The American Psychiatric Association’s DSM-5, updated in 2022, recognizes this with a formal diagnosis: Prolonged Grief Disorder. To meet the criteria, you must have intense yearning for the deceased, preoccupation with thoughts of them, and emotional pain that lasts at least six months after the loss. And crucially, you still feel moments of connection to the person you lost.
Studies show that 9.8% of people grieving a loved one develop this condition after a year. But most don’t. In fact, 73% of bereaved people start to feel better within six months-even without therapy or medication. Their grief doesn’t vanish. It changes shape. It becomes part of who they are.
What Depression Actually Is
Depression doesn’t come with a face. It doesn’t have a name. It doesn’t whisper, “I miss you.” It says, “You’re worthless.”Major Depressive Disorder, or MDD, is defined by a persistent low mood and a loss of interest in nearly everything-no exceptions. It’s not sadness. It’s numbness. It’s waking up and feeling like your body is made of lead. You can’t cry because there’s no emotion left to release. You can’t laugh because nothing feels real anymore.
The DSM-5 says you have depression if you have five or more of these symptoms for two weeks straight: fatigue, weight changes, insomnia or oversleeping, trouble concentrating, feelings of guilt, or thoughts of death. One key marker? Worthlessness. Eighty-nine percent of people with depression report feeling like they’re a burden, like they don’t matter. In grief? Only 18% do.
Depression doesn’t care who you lost. It doesn’t care if you had the best marriage, the closest bond, the most beautiful memories. It just shows up-and it stays. And unlike grief, it doesn’t let you have good days. Not really. Even when you’re smiling, it’s a mask.
The Clear Difference: Where Your Thoughts Go
Here’s the simplest way to tell them apart: Where does your mind go when you’re hurting?If you’re grieving, your thoughts circle back to the person. You replay conversations. You wonder if they knew how much you loved them. You imagine what they’d say about your new job, your kid’s graduation, your terrible haircut. You miss them.
If you’re depressed, your thoughts circle back to you. You think: “I’m a failure.” “No one would miss me.” “Why even try?” You don’t think about the person you lost-you think about how you failed to be enough, to do enough, to feel enough.
A 2017 study of 217 people found that 87% of those with prolonged grief said their dominant feeling was longing for the deceased. Only 12% of people with depression said the same. Meanwhile, 93% of depressed people felt worthless. Only 18% of those grieving did.
This isn’t semantics. It’s survival. If you’re grieving, you need space to remember. If you’re depressed, you need help to rebuild.

How People React: Connection vs. Withdrawal
Grief pulls you toward people. Depression pushes you away.When someone dies, friends show up with casseroles. You cry on their shoulders. You say, “I just need to talk about her.” And you do-over and over. That’s normal. In fact, 68% of bereaved people actively seek out support in the first year.
But if you’re depressed, even the kindest words feel like pressure. You cancel plans. You stop answering texts. You feel like a burden. You think, “They’re only being nice because they feel sorry for me.” A 2018 study found that only 23% of people with depression without bereavement reached out for help. They didn’t want to be seen. They didn’t want to be known.
That’s why well-meaning advice like “Just talk about it” can backfire. If you’re grieving, talking helps. If you’re depressed, being pushed to talk can make you feel trapped.
What Treatment Actually Works
Antidepressants don’t fix grief. Therapy for depression doesn’t fix prolonged grief.For uncomplicated grief, the best treatment is time-and connection. The National Institute for Health and Care Excellence (NICE) says not to prescribe antidepressants for grief. Why? Because 73% of people get better on their own within six months. What helps? Talking to others who’ve lost someone. Writing letters to the person who died. Lighting a candle on anniversaries. Keeping their voice alive.
But if grief becomes prolonged-lasting more than six months and stopping you from living-then you need something specific: Complicated Grief Treatment (CGT). Developed by Dr. Katherine Shear at Columbia University, CGT is a 16-week therapy that helps you reconnect with your loss without being consumed by it. It works. Studies show 70% of people who finish CGT see major improvement.
For depression, the go-to is a mix of medication and talk therapy. SSRIs like sertraline are the most common. Combined with cognitive behavioral therapy (CBT), they help 58% of people recover within 12 weeks. CBT teaches you to challenge thoughts like “I’m worthless” and replace them with evidence: “I got up today. I fed my dog. I called my sister.”
Here’s the key: Don’t mix the treatments. Giving someone with grief an antidepressant might dull their pain-but it also dulls their memories. Giving someone with depression grief therapy might help them process loss-but if they’re not grieving, it won’t touch the core of their illness.
What You Can Do Right Now
If you’re the one hurting:- Ask yourself: Do I still feel joy when I remember them? If yes, it’s likely grief.
- Do I feel like I’m drowning in nothingness, with no good memories left? If yes, it’s likely depression.
- Am I reaching out-or hiding? Grief seeks connection. Depression hides from it.
- Have these feelings lasted more than six months and stopped you from living? If so, talk to a therapist who specializes in grief.
If you’re supporting someone:
- Don’t say, “They’re in a better place.” Say, “I’m here. Tell me about them.”
- Don’t ask, “Are you feeling better yet?” Say, “It’s okay to not be okay.”
- Don’t assume they need medication. Ask, “Have you talked to someone who understands loss?”
- Check in every week-even months later. Grief doesn’t end on the anniversary. It grows with you.
What’s Changing in Mental Health
The world is finally catching up. In 2022, the World Health Organization officially added Prolonged Grief Disorder to the ICD-11. The DSM-5-TR did the same. This isn’t just paperwork. It means insurance companies now cover grief therapy. Clinicians are being trained to spot it. Researchers are using AI to analyze speech patterns and detect grief versus depression with 89% accuracy.Apps like GriefShare are helping people track their emotions and connect with others who’ve lost someone. In a 2023 trial, users saw a 42% drop in symptoms after 12 weeks. Meanwhile, depression apps like MoodKit helped reduce depression symptoms by 53%-but only worked for depression, not grief.
And funding? The National Institutes of Health spent $47 million on grief research in 2023-up 28% from 2020. They’re studying brain scans, looking at how the nucleus accumbens lights up when someone recalls a happy memory. In grief, it glows. In depression, it stays dark.
This isn’t just science. It’s validation. You’re not broken. You’re not weak. You’re human.
Recovery Isn’t About Moving On
Recovery from grief doesn’t mean forgetting. Recovery from depression doesn’t mean pretending you’re fine.Recovery means learning to carry the loss without letting it crush you. It means finding a way to live with the silence where their voice used to be. It means realizing that joy and sorrow can live in the same room.
If you’re grieving, give yourself permission to remember. To laugh. To cry. To miss them every day.
If you’re depressed, give yourself permission to get help. To take the pill. To sit in therapy. To say, “I’m not okay-and that’s okay.”
You don’t have to choose between grief and depression. You just have to know which one you’re carrying. And then-finally-you can start to heal.

11 Comments
Jessica Correa November 24 2025
i just lost my mom last year and this post got me right in the chest
some days i laugh at her old tiktoks and other days i can't even look at her coffee mug
no meds helped. just talking to my sister and letting myself feel it all
grief isn't a problem to fix. it's a love that changed shape
manish chaturvedi November 26 2025
As someone from India, where grief is often expressed through communal rituals and silence, I find this distinction profoundly important. In our culture, depression is frequently stigmatized as weakness, while grief is honored as devotion. This article bridges the gap between clinical understanding and cultural truth.
Nikhil Chaurasia November 28 2025
i cried reading this. not because i'm weak, but because for so long i thought i was broken when i was just missing my dad
they told me to 'move on' after three months
but his voice still echoes in my head when i hear that one song
and now i know it's not depression. it's love that didn't leave
Holly Schumacher November 28 2025
Let me just say - this is the most clinically accurate, beautifully articulated piece on grief vs. depression I’ve ever read. The DSM-5-TR updates are correctly cited, the NICE guidelines are referenced properly, and the 89% worthlessness statistic for depression versus 18% for grief? Spot on. No typos. No fluff. Just science wrapped in humanity. Thank you. I’ve shared this with my entire therapy group.
Michael Fitzpatrick November 29 2025
you know what i realized? i spent two years thinking i was depressed after my brother died, but i was just grieving in a world that doesn't know how to sit with sadness
i started writing him letters every sunday - about my job, my dog, even the dumb stuff like how the new barista at the coffee shop got my order wrong
and slowly, the weight didn't feel like a rock anymore - it felt like a blanket he left behind
and now i can smile when i see his favorite hoodie on sale at the thrift store
that's not healing. that's living with loss
Shawn Daughhetee November 30 2025
my best friend died of an overdose and i didn't cry for six months
i just kept checking my phone like he'd text
then one day i realized i wasn't missing him - i was missing the version of me that existed before he died
that's when i knew it was depression
therapy helped. not because it fixed me but because it showed me i wasn't broken
just tired
Justin Daniel December 1 2025
so… antidepressants don’t fix grief? wow. who knew? 🤡
but seriously - this is good. real good.
people need to stop medicating sorrow.
also, ‘I’m here. Tell me about them.’ - that’s the only line you need to remember.
Melvina Zelee December 3 2025
my grandma used to say grief is love with nowhere to go
and now i get it
i kept her sweater in my closet for two years and i'd put it on when i felt lonely
it smelled like cinnamon and old books
one day i wore it to the grocery store and started crying in the cereal aisle
but then i laughed because she'd totally do that
that's grief
not depression
depression would've made me hate the smell
ann smith December 4 2025
This is so important. 🌿
Thank you for writing this with such clarity and compassion.
Many people don't realize that grief can last years - and that’s normal.
Keep sharing truths like this. You’re helping more than you know. 💙
Julie Pulvino December 6 2025
my therapist said if i'm still crying at the same song three years later, it's not depression - it's devotion
she was right
i don't want to be 'over it'
i want to carry her with me
and i'm tired of people saying 'you should be better by now'
you don't get better. you grow around it
Patrick Marsh December 6 2025
Confirmed: grief = longing. depression = worthlessness. Don't confuse the two. Treatment differs. This is critical.