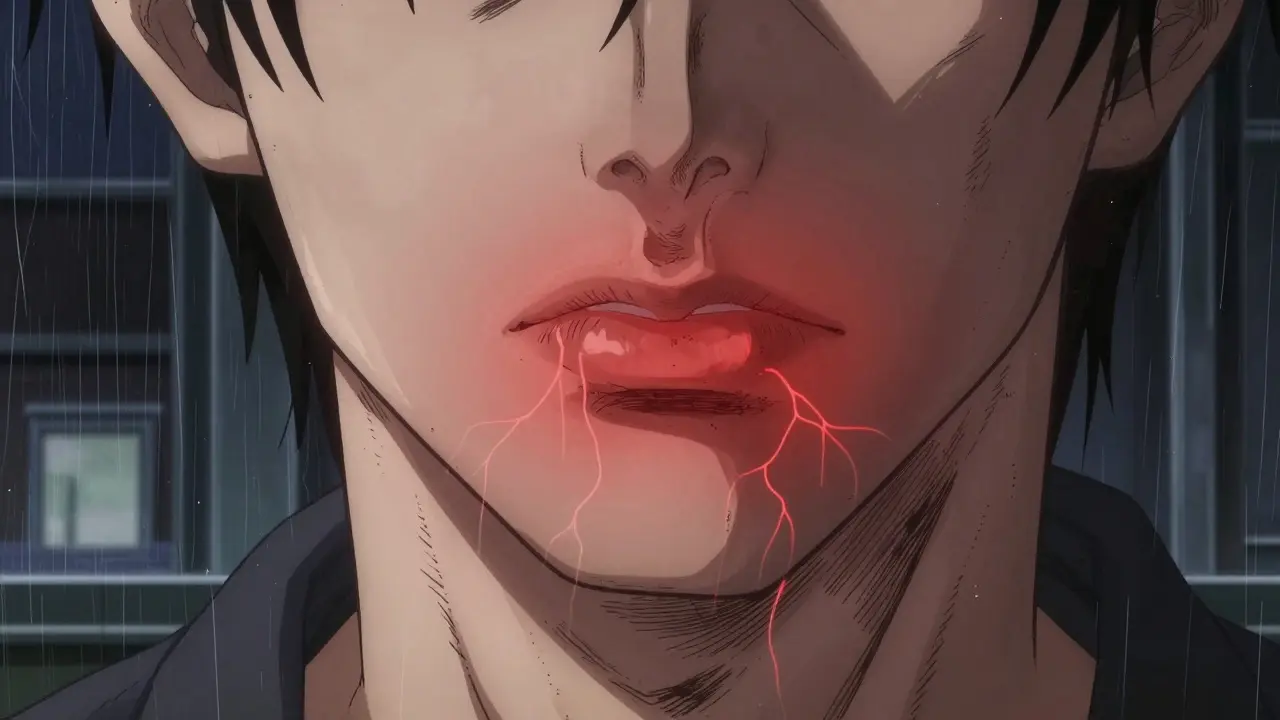
Herpes simplex on the skin isn’t just a rash-it’s a recurring battle. Whether it’s a tingling lip that turns into a cold sore or a cluster of blisters near the genitals, the virus doesn’t go away after the first outbreak. Once it’s in your body, it hides in your nerves and comes back when you least expect it. The good news? You can take real steps to reduce how often it returns and make outbreaks less painful when they do happen.
Why Herpes Keeps Coming Back
The herpes simplex virus (HSV) lives in your nerve cells after your first infection. It stays quiet until something triggers it to wake up. Common triggers include stress, sun exposure, illness, hormonal shifts, and even dental work or laser skin treatments. For some people, outbreaks happen once a year. For others, they show up every few weeks. There’s no single reason why one person gets frequent outbreaks and another rarely does-it’s personal.What Works: Antiviral Medications for Prevention
The most proven way to stop herpes from coming back is daily antiviral medicine. Three drugs are used: acyclovir, valacyclovir, and famciclovir. These aren’t cures-they slow the virus down so it can’t reactivate as easily. Valacyclovir is the most popular choice for prevention because it’s absorbed better than acyclovir. You take it once or twice a day, depending on your needs. For people who have six or more outbreaks a year, daily use cuts recurrences by 70 to 80%. That means going from eight outbreaks a year to one or two. A 2021 Cochrane review of 38 studies confirmed this level of effectiveness. But not everyone needs daily pills. If you only get one or two outbreaks a year, it’s usually not worth the cost or side effects. Instead, use episodic treatment: take the medicine as soon as you feel the first warning signs-tingling, itching, or burning. Starting within an hour of these symptoms can shorten healing time by almost a full day. Waiting until the blister appears? That cuts the benefit in half.When to Take Medicine Before Procedures
If you’re planning a cosmetic procedure like laser skin resurfacing, chemical peel, or even a deep dental cleaning, tell your provider you have herpes. Even if you haven’t had an outbreak in years, the stress of the procedure can trigger one. Studies show that taking valacyclovir 500 mg twice a day for 10 to 14 days before and after laser treatments can prevent outbreaks entirely. In one trial with 120 patients, those who skipped the medicine had a 10-20% chance of getting a lesion. Those who took it? Zero outbreaks. That’s why 87% of U.S. dermatology clinics now require pre-procedure antiviral prophylaxis for patients with a history of herpes.Non-Medical Ways to Reduce Outbreaks
Medication helps, but lifestyle changes make a big difference too.- Sun protection: UV light is a top trigger for cold sores. Use SPF 30+ lip balm every day-even in winter. A 2022 survey of 1,200 people found 76% had fewer outbreaks when they did this consistently.
- Stress management: Stress is the #1 trigger reported by people in online herpes communities. Meditation, regular sleep, and exercise aren’t just good for your mental health-they reduce viral reactivation.
- Zinc supplements: Taking 15-30 mg of zinc daily may reduce the severity and duration of outbreaks. One study showed zinc lozenges helped sores heal faster when used at the first sign of tingling.
- Avoid triggers: If you notice outbreaks happen after drinking alcohol, eating chocolate, or getting sick, track it. Avoiding those triggers can help.

What Doesn’t Work
There’s a lot of misinformation out there. Don’t waste time or money on things that don’t help:- Topical creams (like acyclovir ointment): Applying cream to a cold sore won’t stop future outbreaks. It might ease pain a little, but it doesn’t reduce recurrence.
- Essential oils or home remedies: Tea tree oil, lemon balm, or lysine supplements have weak or no scientific backing for preventing outbreaks. Some may even irritate your skin.
- Only treating after the sore appears: If you wait until you see a blister, you’ve already missed the best window to stop it from getting worse.
Cost and Side Effects
Antiviral meds aren’t cheap. In the U.S., valacyclovir can cost $370 a month without insurance. That’s why many people skip doses. In a 2022 survey, 72% of respondents admitted they didn’t take their pills regularly because of cost. If you’re struggling, ask your doctor about generic versions or patient assistance programs. Side effects are usually mild: headache, nausea, or dizziness. Long-term use can affect kidney function, especially in older adults or people with existing kidney issues. Your doctor should check your creatinine clearance before prescribing daily antivirals.Can You Stop Transmission?
Yes-but not completely. Daily antiviral therapy reduces the chance of passing HSV to a partner by about half. A 2004 study showed a 48% drop in transmission with daily valacyclovir. But even with medication, about 4-5% of serodiscordant couples still see transmission over time. That’s why using condoms and avoiding sex during outbreaks is still critical.
What About a Vaccine?
There’s no approved vaccine yet. Two candidates-GEN-003 and HSV529-were tested in 2022-2023 and showed only modest results. They reduced viral shedding slightly but didn’t prevent outbreaks. Research continues, but don’t count on a vaccine anytime soon.When to See a Doctor
You don’t need to wait until you’re in pain. Talk to a provider if:- You have more than six outbreaks a year
- Outbreaks last longer than two weeks
- You’re having outbreaks near your eyes
- You’re pregnant or planning to be
- You’re immunocompromised
Real Stories, Real Results
One woman from New Zealand started getting cold sores every time she traveled. After switching to daily valacyclovir and using SPF lip balm religiously, she went from 10 outbreaks a year to just one in two years. She says the peace of mind was worth the cost. Another man with genital HSV-2 used to feel ashamed to date. After starting suppressive therapy, his outbreaks dropped from eight a year to one. He says he finally felt like he could be open with partners.What to Do Next
Start by tracking your outbreaks. Note when they happen, what you were doing, and how you felt. That pattern will tell you your triggers. Then talk to your doctor about whether daily antivirals make sense for you. If not, focus on sun protection, stress reduction, and starting treatment early when you feel the first signs. Herpes won’t disappear. But with the right plan, it doesn’t have to control your life.Can herpes simplex be cured?
No, herpes simplex virus cannot be cured. Once infected, the virus stays in your nerve cells for life. But it can be managed effectively with antiviral medications, trigger avoidance, and good skin care. Most people with HSV live normal, healthy lives without frequent outbreaks.
How do I know if I’m having a prodrome?
The prodrome is the early warning stage before a visible sore appears. Signs include tingling, burning, itching, or numbness in the area where the outbreak usually happens-like your lip, chin, or genitals. These symptoms can last a few hours to two days. Learning to recognize your prodrome is the most important step in using episodic treatment effectively.
Is it safe to take antivirals long-term?
Yes, for most people. Acyclovir, valacyclovir, and famciclovir have been used safely for decades. Long-term use is monitored by checking kidney function, especially in older adults or those with existing kidney disease. If your creatinine clearance is above 50 mL/min, daily use is generally safe. Always follow your doctor’s advice and get regular blood tests if you’re on suppressive therapy for more than a year.
Can I still have sex if I have herpes?
Yes, but with precautions. Avoid sexual contact during outbreaks and when you feel prodrome symptoms. Use condoms and dental dams even when you feel fine-they reduce but don’t eliminate risk. Daily antiviral therapy cuts transmission risk by about half. Open communication with partners is key. Many people with HSV have healthy, long-term relationships.
Do I need to tell my dentist or dermatologist I have herpes?
Yes. Any procedure that causes stress to the skin or mucous membranes-like laser treatments, chemical peels, or deep dental work-can trigger an outbreak. If you’ve had herpes before, your provider should know so they can prescribe preventive antivirals. This is now standard practice in most clinics.
What if I can’t afford the medication?
Ask your doctor about generic versions. Acyclovir is much cheaper than valacyclovir and still effective for episodic use. Some pharmacies offer discount programs, and pharmaceutical companies have patient assistance plans. In New Zealand, publicly funded prescriptions may cover part of the cost. Don’t skip doses because of cost-talk to your provider. They may adjust your plan to fit your budget.
Can stress really cause herpes outbreaks?
Yes. Stress affects your immune system, which lets the virus reactivate. In online communities, 68% of people report stress as their main trigger. Managing stress through sleep, exercise, or therapy can reduce outbreaks just as much as medication for some people.
Is herpes only spread through sex?
No. HSV-1, which causes cold sores, is often spread through kissing, sharing utensils, or towels. HSV-2 is mostly genital and spread through sexual contact. But both types can infect either area. You can get genital herpes from oral sex if your partner has a cold sore. Always avoid contact during outbreaks and be aware that shedding can happen even without symptoms.
Do I need to tell my partner I have herpes?
Yes. Ethically and legally, you should disclose your status before sexual contact. It’s not about shame-it’s about informed consent. Many partners are understanding, especially if you’re on suppressive therapy and use protection. Support groups and counselors can help you prepare for this conversation.
Will herpes affect my ability to have children?
Not if managed properly. If you’re pregnant and have herpes, your doctor will monitor you closely. If you have an outbreak near your due date, a C-section may be recommended to prevent passing the virus to your baby during delivery. But most women with HSV have healthy vaginal deliveries. The key is early prenatal care and open communication with your provider.
Herpes is common. It’s manageable. And with the right approach, you can live well despite it.
15 Comments
Aparna karwande January 6 2026
This article is a godsend. I’ve been dealing with cold sores since I was 12, and no one ever told me about the prodrome or how to use antivirals early. I started taking valacyclovir at the first tingle last month-no outbreak. I’m not exaggerating when I say this changed my life. No more hiding behind scarves in winter. No more panic before dates. Just peace.
Also, SPF lip balm? Non-negotiable. I used to think it was just for beach days. Turns out, my office window is a herpes trigger. Who knew?
And yes, I’m still mad about the $370/month price tag. But I’d rather pay than suffer.
Thank you for writing this with actual science, not snake oil.
Ayodeji Williams January 7 2026
bro i got herpes from my ex who said she was ‘clean’ 😭
now i can’t even kiss my new gf without anxiety
and don’t even get me started on dental work 😵💫
but tbh the meds helped a lil
still feel like a leper tho 💔
Kyle King January 7 2026
Let me guess-this was written by Big Pharma. Daily antivirals? 70-80% reduction? Sounds like a scam to keep you hooked. The virus doesn’t ‘hide in nerves’-that’s a myth created to sell pills. Real healers use lysine, zinc, and sunlight. The CDC’s been lying to us since the 90s. They don’t want you cured-they want you medicated for life. And don’t get me started on the ‘no vaccine’ thing. There’s one. It’s just banned. Ask about HSV-529. They buried it.
They’re scared of what happens when people stop paying for this scam.
Vince Nairn January 8 2026
So you’re telling me I’ve been doing it wrong my whole life?
I used to wait until the blister popped before I took anything. I thought that was the ‘right’ time. Turns out I was just giving the virus a head start.
Also, I didn’t know laser treatments could trigger it. I got a facial last year and ended up with a whole face full of sores. Now I know why.
Thanks for the clarity. I’m calling my doc tomorrow.
Also, SPF lip balm. I’ll start using it. Even if I look like a sunscreen zombie in winter. Worth it.
Mina Murray January 8 2026
So let me get this straight-you’re telling me to take a drug for the rest of my life because some virus is ‘hiding’ in my nerves? Sounds like a sci-fi movie plot. And why do they say it’s ‘manageable’? That’s just corporate speak for ‘you’ll never be free.’
And SPF? Are you kidding me? I’ve had outbreaks in the winter. In a basement. No sun. So why is that even a trigger? Someone’s lying. Either the science is fake or they’re hiding something. Also, why is valacyclovir so expensive? Because it’s patented. And why is it patented? Because someone owns the cure and they don’t want you to have it.
And don’t even get me started on ‘open communication with partners.’ That’s just guilt-tripping. What if I don’t want to tell anyone? Why is it my burden to carry?
I’m not buying it.
Jessie Ann Lambrecht January 8 2026
I’m a nurse and I’ve seen so many patients suffer in silence because they’re ashamed. This post? It’s everything. No shame. No stigma. Just facts.
One of my patients, a 72-year-old woman, had been having outbreaks every 3 weeks. She thought it was ‘just bad luck.’ After starting daily valacyclovir and using SPF lip balm religiously? One outbreak in 18 months. She cried when she told me.
And yes, stress is a monster. One of my patients started yoga and cut out alcohol-and her outbreaks dropped from 10 a year to 2. No meds needed.
Don’t let anyone make you feel broken. This virus doesn’t define you. You’re still you. Still lovable. Still worthy.
And if cost is a problem? Ask for generics. Ask for help. You’re not alone.
Kamlesh Chauhan January 9 2026
all this talk about meds and sunblock and stress
why not just say the truth
its a curse
you got it
you live with it
the rest is just noise
you think you’re in control
but the virus wins when you’re tired
when you’re sad
when you forget to take your pill
so yeah
take the meds
use the balm
but don’t pretend it’s not a life sentence
you’re just buying time
and the virus? it’s just waiting
Christine Joy Chicano January 10 2026
Can we talk about the emotional toll? It’s not just the physical outbreaks-it’s the fear. The dread before a date. The panic when you feel a tingle. The guilt when you think you might’ve passed it on. The way you start avoiding mirrors because you don’t want to see it.
I used to think I was the only one who cried after an outbreak. Turns out, everyone does. We just don’t talk about it.
This article didn’t just give me medical advice-it gave me permission to stop hiding. To stop apologizing. To stop believing I was broken.
Thank you. I needed this.
Rachel Steward January 10 2026
Here’s the uncomfortable truth: herpes isn’t a medical condition. It’s a social one.
It’s not the virus that shames you-it’s the stigma. The way people whisper. The way partners ghost. The way doctors say ‘it’s manageable’ like that’s enough.
We treat herpes like a moral failure. Like you did something wrong. Like you’re dirty. But it’s just a virus. It doesn’t care about your job, your worth, your love life. It just wants to replicate.
And yet, we’ve turned it into a character flaw. We make people feel like they’re less than because of a microscopic invader that lives in their nerves.
Maybe the real cure isn’t a pill.
Maybe it’s a culture that stops treating people like pariahs.
Until then, we’re all just buying time.
Emma Addison Thomas January 12 2026
Coming from the UK, I’m grateful this was written so clearly. Here, many GPs still treat herpes like a taboo. I had to push for valacyclovir for months. My doctor said, ‘It’s just a cold sore.’
But it’s not just a cold sore. It’s a recurring trauma. It’s the way you avoid kissing your niece because you’re scared. It’s the way you panic before a job interview because your lip is tingling.
I’m glad the article mentions dental work. I had a root canal last year and got an outbreak on my chin. No one asked if I had HSV. No one warned me.
Knowledge is power. And this article gave me power.
Thank you.
Adam Gainski January 13 2026
I’ve been on daily valacyclovir for three years. Outbreaks? One every 18 months. And I still forget to take my pill sometimes. Life happens.
But here’s what I learned: it’s not about perfection. It’s about progress.
I used to think I had to be flawless-no stress, no sun, no alcohol, no sleepless nights. But that’s impossible. So I stopped trying to control everything.
I started focusing on what I could control: taking the pill, using SPF, and talking to my partner honestly.
And that’s enough.
You don’t need to be perfect. You just need to keep showing up.
And you’re not alone.
Anthony Capunong January 14 2026
Wow, so now I’m supposed to take pills forever because I got herpes from my ex? And I’m supposed to feel bad about it? I’m American. We don’t take drugs for life unless we’re dying. This is a weak excuse to make people pay for meds.
Also, why is everyone so obsessed with ‘transmission’? It’s just a virus. I’ve had sex with 20 people and never told any of them. They’re fine. They’re still alive.
And SPF lip balm? I don’t even go outside. I live in a cave. So why am I paying for this nonsense?
This is just fear-mongering dressed up as science.
Alex Danner January 15 2026
Just wanted to add one thing: the 2021 Cochrane review didn’t just look at valacyclovir-it compared all three antivirals. Acyclovir is just as effective if you take it 5x a day. But nobody wants to do that. So they push valacyclovir because it’s once or twice daily.
Also, zinc lozenges? They work best when dissolved slowly in your mouth, not swallowed. Most people use them wrong.
And yes, the cost is insane. But in Canada, it’s $15/month. In India, it’s $3. In the US? $370. That’s not a medical issue. That’s a capitalism issue.
Stop blaming the virus. Start blaming the system.
Jonathan Larson January 17 2026
Herpes is not a punishment. It is not a moral failing. It is not a reflection of your character.
It is a biological event-a viral colonization that occurred in your youth, likely before you understood consent, boundaries, or even what a condom was.
It does not diminish your capacity for love. It does not make you unworthy of intimacy. It does not make you less than.
The real tragedy is not the virus.
The real tragedy is the silence we’ve imposed upon those who carry it.
This article is a quiet revolution. It offers not just treatment, but dignity.
Thank you for speaking truth into the noise.
Elen Pihlap January 18 2026
so i got herpes and now i can’t even kiss my dog??