Every year, hundreds of thousands of people in the U.S. get the wrong medication, the wrong dose, or incorrect instructions at the pharmacy. Many of these mistakes aren’t caused by reckless pharmacists-they happen because the system relies on one person to catch errors, and humans make mistakes. You can’t control the pharmacy’s workflow, but you can control what you do when you walk up to the counter. A simple personal safety checklist for pharmacy visits isn’t just a good idea-it’s a lifeline.
Why Your Pharmacy Visit Needs a Checklist
You don’t need to be a medical expert to spot a dangerous mistake. A 2022 study from the Institute for Safe Medication Practices found that over 40% of dispensing errors could have been caught by the patient if they’d asked two simple questions. That’s not luck. That’s awareness. Most people assume the pharmacy has already double-checked everything. But pharmacies are busy. One pharmacist might be filling 30 prescriptions at once. A label might be misprinted. A computer might swap two similar-looking drugs-like hydrocodone and hydromorphone. These aren’t rare mistakes. They happen daily. Your job isn’t to be a pharmacist. Your job is to be a second set of eyes. You’re not replacing the system-you’re reinforcing it.The Five-Step Personal Safety Checklist
Here’s what you should do every single time you pick up a prescription. No exceptions.- Confirm the patient name-out loud. Don’t just nod. Say: “Is this for [Your Full Name]?” Pharmacists hear names all day. They might misspell yours, mix you up with someone else, or hand you the wrong bag. Hearing your name spoken back confirms you’re getting your meds.
- Check the drug name and strength-compare it to your prescription. If your doctor prescribed metformin 500 mg, but the bottle says metformin 1000 mg, that’s not a typo-it’s a risk. Ask: “Is this the same as what my doctor ordered?” Keep a copy of your prescription on your phone or in your wallet. You don’t need to memorize it.
- Verify the dosage instructions-out loud again. The label might say “Take one tablet twice daily,” but your doctor meant “Take one tablet with breakfast and dinner.” Don’t assume. Say: “So I take this in the morning and at night, right?” If the instructions are unclear, ask for clarification. Never guess.
- Look for changes-in color, shape, size, or markings. If you’ve taken this drug before, you know what it looks like. If the pill is now blue instead of white, or has a different imprint, ask: “Is this the same medicine I got last time?” Generic drugs can look different, but you should still be alerted if something feels off.
- Ask about interactions-even if you’re not sure. Say: “Could this interact with anything else I’m taking?” List your other meds, supplements, or even over-the-counter painkillers. Pharmacists are trained to catch dangerous combinations-like warfarin and ibuprofen, or statins and grapefruit juice. You don’t need to know the science. Just ask.
What to Bring to Every Visit
You can’t do this checklist without the right tools. Here’s what to carry every time:- A current list of all your medications (prescription, OTC, supplements)
- The prescription slip or a photo of it from your doctor
- Your phone with your pharmacy’s contact info and your doctor’s number
- A small notebook or notes app to write down instructions
- Any recent lab results if you’re on blood thinners, diabetes meds, or kidney-affecting drugs
Many people think they don’t need this because they’ve been taking the same pill for years. But medications change. Your body changes. Your other drugs change. A new interaction can appear overnight.
Red Flags You Can’t Ignore
If any of these happen, don’t walk away. Stop. Ask. Demand clarification.- The pharmacist says, “It’s fine,” but won’t show you the label or explain why.
- The bottle has no label, or the label is smudged, torn, or handwritten.
- You’re handed a new drug you’ve never seen before, and no one explains why.
- The dosage is different from your last refill without a doctor’s note.
- You’re told, “We’re out of your usual brand,” but no one tells you if the generic is safe to switch.
These aren’t minor issues. They’re warning signs. One pharmacy error led to a 68-year-old woman taking 10 times her prescribed dose of insulin. She went into a coma. She survived. But she didn’t catch it herself. She trusted the system.
What to Do If You Spot an Error
If you notice something wrong, don’t panic. Don’t argue. Just say:“I think there might be a mistake. Can we double-check this?”
Most pharmacists will thank you. They want to get it right. If they brush you off, ask to speak to the manager. If they still won’t help, call your doctor. Take a photo of the label. Write down the date, time, pharmacy name, and pharmacist’s name (if possible). Then file a report with the FDA’s MedWatch program-it’s online, free, and anonymous.
Why This Works Better Than You Think
You might think, “I’m just one person. What difference can I make?”Here’s the truth: pharmacists want patients to ask questions. A 2023 survey by the American Pharmacists Association found that 87% of pharmacists said patients who ask about their meds are more likely to take them correctly-and fewer make mistakes.
When you ask questions, you’re not being difficult. You’re helping the system work better. You’re reducing the chance that the next person gets your error.
What You Shouldn’t Do
Don’t assume. Don’t rush. Don’t feel bad for asking.- Don’t skip the checklist because you’re in a hurry. The faster you are, the more likely you are to miss something.
- Don’t let embarrassment stop you. Pharmacists hear “What does this pill do?” 50 times a day. They’re used to it.
- Don’t rely on memory. Even if you’ve taken this drug for 10 years, write it down. Memory fails. Labels don’t.
Real Example: How a Checklist Saved a Life
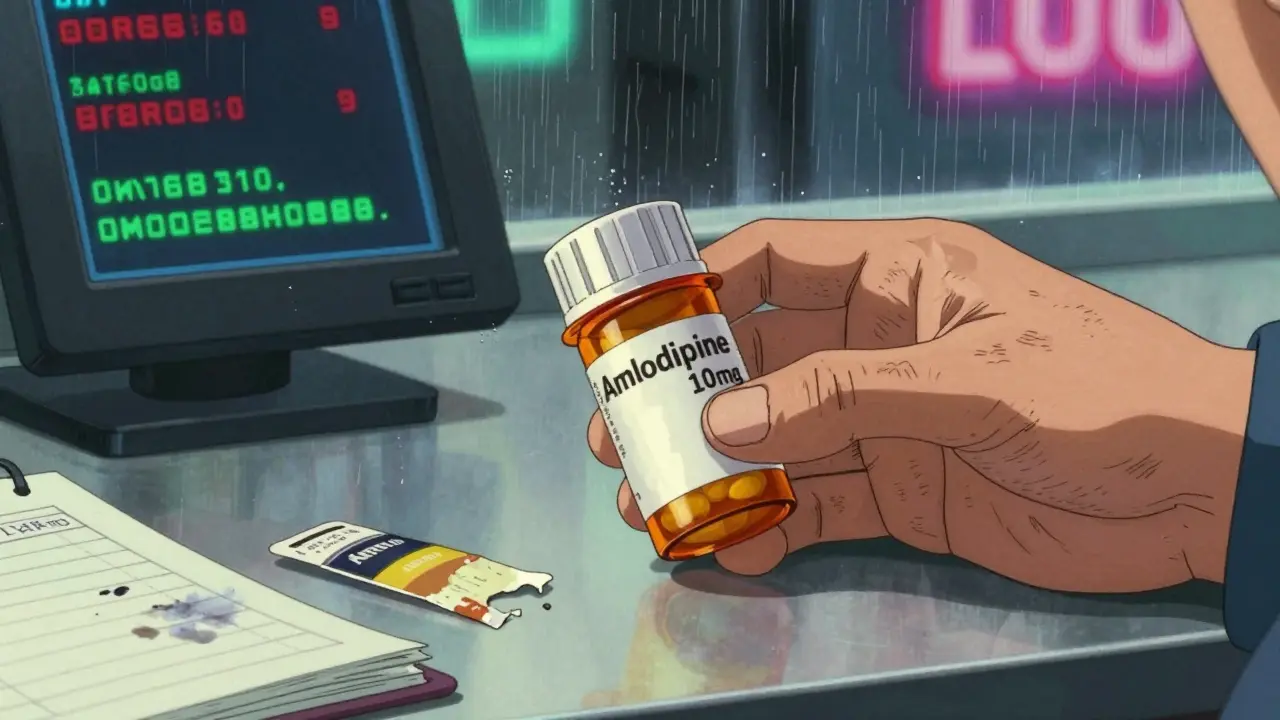
A 72-year-old man in Ohio picked up his new blood pressure med. He’d been on the same one for years. This time, the pill looked different. He didn’t recognize it. He pulled out his phone, opened his doctor’s email, and compared the label. The new drug was amlodipine, but the dose was 10 mg instead of 5 mg. He asked the pharmacist. The pharmacist checked the system-there had been a computer glitch. The wrong dose had been sent. The man didn’t take it. He called his doctor. A serious overdose was prevented.He didn’t know pharmacology. He just had a checklist.
Next Steps: Build Your Personal Safety Routine
Start today. Print out this checklist. Put it on your fridge. Save it in your phone. Use it every time.Make it a habit. After a few visits, it’ll feel automatic. And when it does, you’ll realize something important: you’re not just protecting yourself. You’re helping everyone around you.
Medication safety isn’t just the pharmacy’s job. It’s your job too.
Can I really trust my pharmacist if I ask questions?
Yes. Pharmacists are trained to answer questions-and they appreciate patients who ask. A 2023 survey of over 1,200 pharmacists found that 9 out of 10 said patients who ask about their meds are more likely to take them correctly. Asking isn’t a sign of distrust. It’s a sign of smart self-care.
What if the pharmacy refuses to correct a mistake?
If a pharmacist dismisses your concern, ask to speak to the manager. If that doesn’t work, call your doctor and explain what happened. Take a photo of the incorrect label, note the date and pharmacy name, and report it to the FDA’s MedWatch program. You have the right to safe medication. No pharmacy should make you feel wrong for protecting yourself.
Do I need to check every prescription, even if it’s the same as last time?
Yes. Even if you’ve taken the same drug for years, the manufacturer, dosage, or formulation can change. Generic drugs look different. Doses get adjusted. A small change can be dangerous. Always verify. It takes 30 seconds. That’s less time than it takes to scroll through your phone.
Can I use this checklist for over-the-counter meds too?
Absolutely. OTC drugs like painkillers, sleep aids, or allergy meds can interact with your prescriptions. Taking too much acetaminophen can damage your liver. Mixing antihistamines with blood pressure meds can cause dizziness or falls. Always check the label and ask if you’re unsure-even if you bought it without a prescription.
What if I’m elderly or have trouble reading labels?
Ask the pharmacist to read the label aloud to you. Most pharmacies offer this service. You can also bring a family member or caregiver with you. Many pharmacies have large-print labels or audio instructions available upon request. Don’t be afraid to ask for help. Your safety matters more than pride.
