Statin Muscle Cramp Symptom Checker
Your Symptoms
Additional Information
Your Likely Condition
Many people on statins start noticing muscle cramps, aches, or tingling and wonder: is this normal, or is something serious going on? The truth is, not all muscle discomfort from statins is the same. Some is muscle damage - called myopathy. Others may be nerve-related - known as neuropathy. And confusing the two can lead to the wrong decision: stopping a life-saving drug, or keeping one that’s hurting you.
What Statin Muscle Cramps Really Look Like
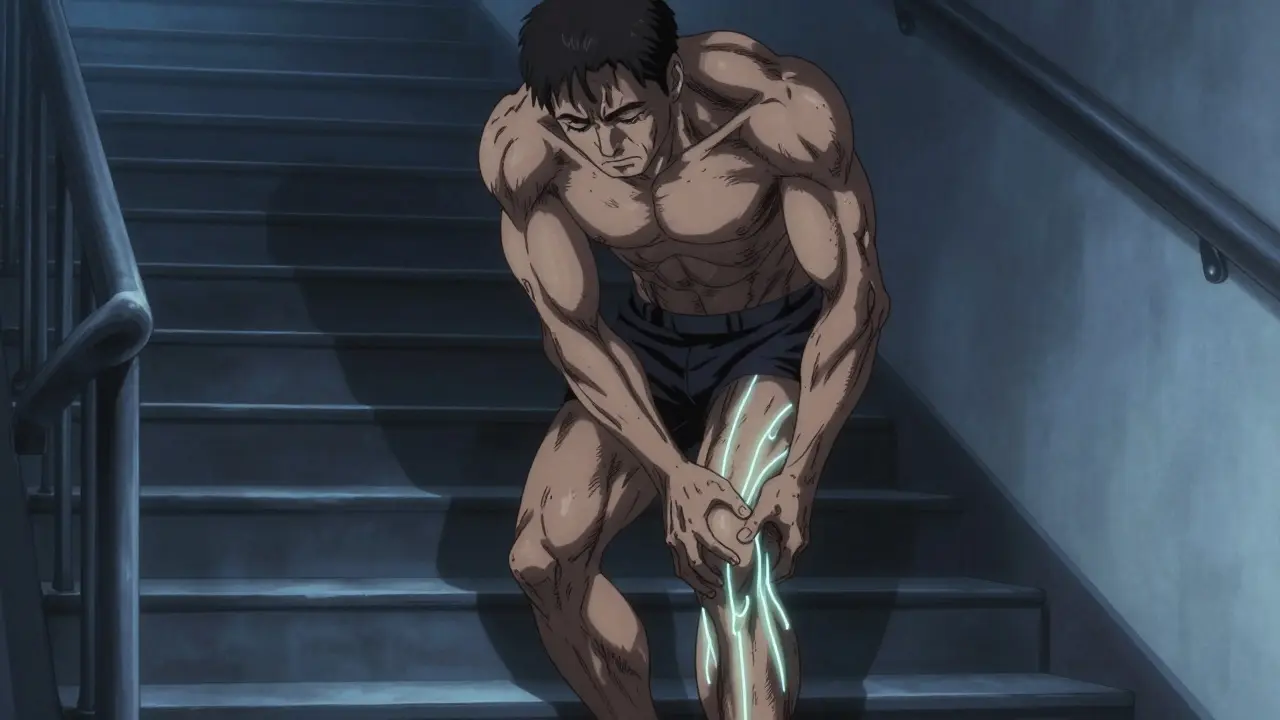
Statins lower cholesterol by blocking an enzyme your liver needs to make it. But that same enzyme is also involved in making coenzyme Q10, which your muscles use for energy. When that drops - by up to 40% in the first month - your muscles start struggling. This is why muscle pain or cramps are the most common complaint among statin users. Studies show 7% to 29% of people on statins report muscle symptoms, but only a tiny fraction have true muscle damage. The key is knowing what kind of pain you’re feeling. If your thighs, hips, or shoulders feel heavy, weak, or sore - especially when climbing stairs or getting up from a chair - that’s classic myopathy. It’s not sharp. It’s not burning. It’s a deep, dull ache that creeps in slowly. You might not even realize your balance is off or you’re walking slower. Doctors often miss this because patients think it’s just aging.Myopathy vs. Neuropathy: The Clues That Matter
Here’s how to tell them apart, side by side:| Feature | Statin Myopathy | Statin-Related Neuropathy |
|---|---|---|
| Location | Proximal muscles (hips, thighs, shoulders) | Distal nerves (feet, hands - stocking-glove pattern) |
| Symptoms | Weakness, heaviness, cramping | Tingling, burning, numbness, pins and needles |
| CK Levels | Often elevated (especially if severe) | Normal |
| Nerve Tests | Normal | Reduced sensory nerve signals |
| Timing | Starts within weeks to months of starting statin | Usually takes over a year to develop |
| Improves After Stopping? | Yes, usually within weeks | Unclear - may not improve even after stopping |
One big red flag: if your feet feel like they’re wrapped in cling film, or you can’t feel your toes when walking barefoot, that’s not myopathy. That’s neuropathy. But here’s the twist - the evidence that statins cause neuropathy is messy. Some studies say yes. Others, like a 2019 study of over 600 people, found statin users had lower rates of neuropathy than non-users. Why? Maybe statins protect nerves by reducing inflammation or stabilizing blood vessels. Or maybe the symptoms people report aren’t really from statins at all.
Why Creatine Kinase (CK) Matters
Your doctor might order a blood test for creatine kinase - a protein that leaks out when muscle cells break down. If your CK is more than four times the normal level, that’s a clear sign of statin myopathy. But here’s the catch: most people with statin muscle pain have normal or only slightly raised CK. That doesn’t mean it’s not real. It just means the damage isn’t severe enough to spill large amounts of protein into the blood. That’s why doctors can’t rely on CK alone. They have to look at your symptoms, your timeline, and what happens when you stop the drug. If your cramps vanish within a few weeks after stopping the statin, and come back when you restart it, that’s diagnostic. This is called a rechallenge - and it’s the gold standard for confirming statin myopathy.What About Neuropathy? Is It Real?
Some patients swear their feet started tingling after being on statins for years. But before jumping to conclusions, rule out the usual suspects: diabetes, low B12, alcohol use, or even spinal issues. These are far more common than statin-induced nerve damage. Even if you have neuropathy and take statins, it doesn’t mean the statin caused it. In fact, some experts think statins might actually help prevent nerve damage. Cholesterol is a building block for nerve membranes. But statins don’t strip away all cholesterol - they just lower the bad kind. And vitamin E, which protects nerves, is carried by LDL. Lower LDL might mean less vitamin E delivery - but again, studies don’t consistently show this leads to nerve problems. Bottom line: if your symptoms match neuropathy, don’t assume it’s the statin. Get tested. Nerve conduction studies can show if there’s real nerve damage - and what kind. If the test is normal, your tingling might be stress, poor circulation, or something else entirely.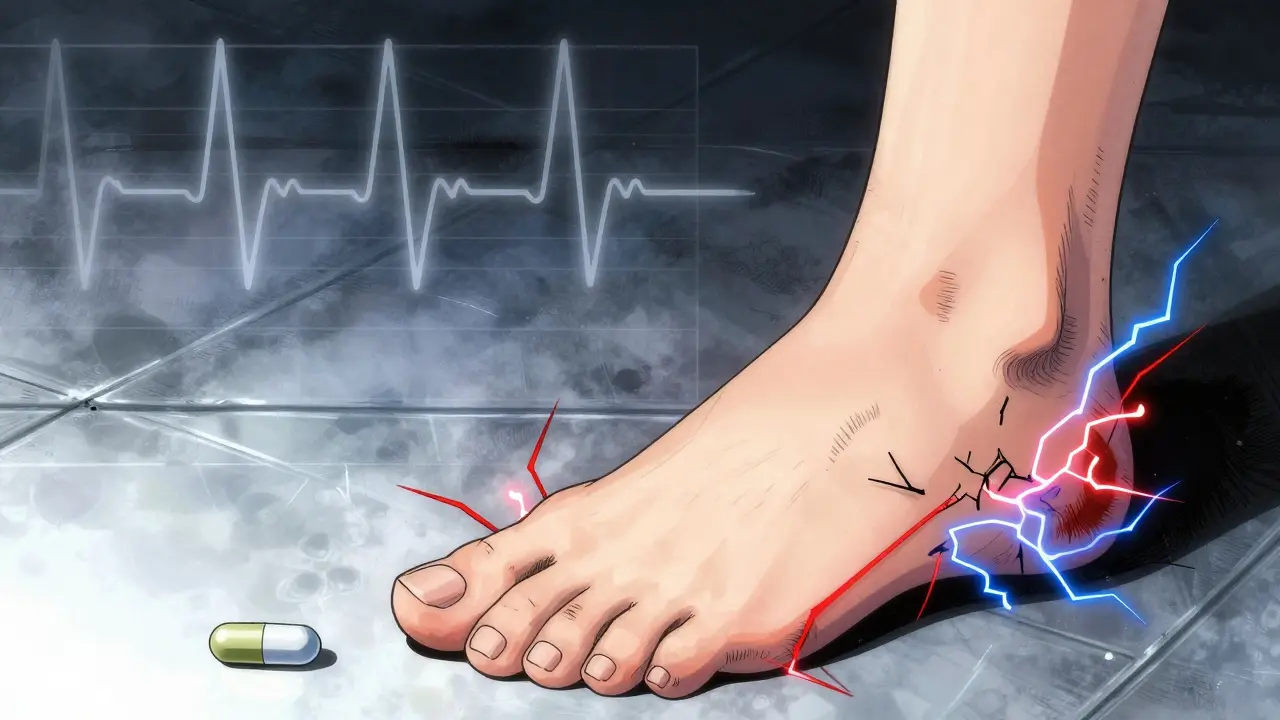
What to Do If You Have Muscle Cramps
Don’t stop your statin on your own. That’s risky. Cardiovascular disease is still the number one killer. Stopping your statin without a plan could mean a heart attack or stroke down the road. Here’s what to do instead:- Track your symptoms. When did they start? What makes them better or worse?
- See your doctor. Ask for a CK test and a basic metabolic panel (to check kidney and thyroid function - both can mimic muscle pain).
- If CK is high or symptoms are strong, pause the statin for 2-4 weeks. See if you feel better.
- If symptoms improve, restart the same statin. If they come back, you’ve confirmed statin myopathy.
- If symptoms don’t improve after stopping, see a neurologist. You might have an unrelated nerve issue that was masked before.
Some people think switching statins helps. And it often does. Hydrophilic statins like pravastatin and rosuvastatin are less likely to enter muscle cells, so they cause fewer muscle problems. About 60% of people who couldn’t tolerate one statin can handle another.
Alternatives If You Can’t Tolerate Statins
If you truly can’t take any statin, you still have options. The goal isn’t to avoid statins - it’s to keep your LDL cholesterol low. The Cholesterol Treatment Trialists’ meta-analysis showed that for every 1 mmol/L drop in LDL, your risk of heart attack or stroke drops by 25%. Non-statin options include:- Ezetimibe: Blocks cholesterol absorption in the gut. Works well with or without statins.
- PCSK9 inhibitors (alirocumab, evolocumab): Injectables that slash LDL by 60% or more. Used for high-risk patients.
- Bempedoic acid: A newer pill that works like a statin but stays in the liver, avoiding muscle exposure.
None of these are perfect. But they’re better than doing nothing. And unlike statins, they don’t carry the same muscle risks.
Supplements? CoQ10, Vitamin E, or Magnesium?
You’ve probably heard about CoQ10. Statins lower it. So, taking a supplement should help, right? A 2015 JAMA study gave CoQ10 to 44 people with statin-related muscle pain. Half got placebo. After 30 days, there was no difference. CoQ10 didn’t help. Same goes for vitamin E and magnesium. No strong evidence they fix statin muscle issues. That doesn’t mean they’re harmful - but don’t waste money hoping they’ll solve the problem. Focus on the right diagnosis instead.
14 Comments
Adewumi Gbotemi January 10 2026
Man, this is the clearest explanation I’ve ever read on statin muscle stuff. I’ve been on them for 5 years and thought my leg cramps were just getting old. Turns out it was dehydration and low vitamin D. Simple fixes, big difference. Thanks for the clarity.
Priscilla Kraft January 11 2026
Thank you for writing this 💪❤️ I was about to quit my statin after 3 months of cramps. Got my CK checked - normal. Started walking daily and stretching before bed. Cramps cut in half. You saved me from a dumb decision. 🙏
Jason Shriner January 13 2026
so like… statins cause myopathy? or maybe not? or maybe they dont? or maybe they do but only if you’re a woman over 65 who also drinks kombucha and believes in chakras? i mean… the science is just… vibes at this point
Matthew Miller January 13 2026
Why are people still wasting time on this? If your CK is normal and you're not turning urine black, you're not in danger. Stop overthinking. Statins save lives. Your 'cramps' are probably from sitting too much and eating too much sugar. Fix your lifestyle before blaming Big Pharma.
Vincent Clarizio January 14 2026
Let’s be real - the entire medical establishment is terrified of admitting that statins cause neurological side effects because the pharmaceutical industry is too powerful. CoQ10 doesn’t work? Of course not - because they don’t want you to know the real solution. The truth is, statins strip your body of cholesterol, which is the literal building block of every nerve cell. You think your tingling feet are ‘stress’? No. Your axons are starving. And they’re covering it up with ‘normal CK’ and ‘maybe it’s diabetes’ because it’s easier than admitting they poisoned you with a pill they profit from. Wake up.
Jennifer Littler January 16 2026
As a neurologist, I see this frequently. Statin-induced neuropathy is exceedingly rare. Most patients presenting with distal paresthesias have undiagnosed prediabetes or vitamin B12 deficiency. I always order HbA1c and serum B12 before even considering statin attribution. The timeline matters - if symptoms began within 3 months, myopathy is more likely. Beyond 12 months, look elsewhere. Don’t self-diagnose. Get the labs.
Christian Basel January 16 2026
Wow. So you’re saying we should just trust the doctor and not question the statin? That’s the same logic they used with thalidomide and Vioxx. If you’re not getting a nerve conduction study and a genetic panel for SLCO1B1, you’re not doing your due diligence. This article is dangerously simplistic. People die from rhabdo. But they also die from ignoring subtle neuropathy. It’s not either/or. It’s both. And you’re reducing it to a checklist.
Sean Feng January 17 2026
CK test. Stop. Go. Done. If it’s high, stop the statin. If it’s not, you’re fine. Stop overcomplicating. You’re not a biochemist. Your doctor isn’t either. Just do the test.
Priya Patel January 17 2026
OMG I thought I was the only one 😭 I’ve been on rosuvastatin for 4 years and my feet felt like they were in socks made of plastic. I thought it was my shoes. Then I read this and got a nerve test - turns out it was just low B12. Took supplements for 2 months and now I can feel my toes again. Thank you for this!! 🙌
Roshan Joy January 18 2026
From India - we don’t have easy access to CK tests or PCSK9 inhibitors here. But we do have garlic, turmeric, and walking 6 km a day. My dad’s LDL dropped from 190 to 130 without statins. Not perfect, but better than nothing. Sometimes the simplest things work. 🙏
Alex Smith January 20 2026
So… if CoQ10 doesn’t work, and vitamin E doesn’t work, and magnesium doesn’t work… what’s left? Just suffer? Or switch to ezetimibe? Because honestly, if I had to choose between a 2% higher heart attack risk and numb toes, I’d pick the numb toes. At least I can still feel my dog’s lick.
Michael Patterson January 20 2026
Guys. You’re all missing the point. The real issue is that statins are being prescribed to people who don’t need them. Like, your LDL is 130 and you’re 45 and you jog once a month? You’re not at risk. You’re just a walking pharmacy ad. Stop blaming the drug. Blame the system that pushes pills like candy.
Madhav Malhotra January 22 2026
As an Indian guy who’s been on statins since 35 - I get it. We don’t talk about side effects here. But I told my doctor about the cramps. He switched me to pravastatin. No more issues. Sometimes it’s just the right statin, not the wrong drug. Keep talking. Don’t suffer in silence.
Alfred Schmidt January 22 2026
STOP. JUST STOP. You people are so obsessed with your ‘tingling toes’ and ‘cramps’ that you’re ignoring the fact that 80% of heart attacks happen in people who were never on statins because they thought they were ‘fine’. Your leg cramps are a tiny price to pay for not dying at 52. If you can’t handle a little discomfort, maybe you shouldn’t be the one making medical decisions. Go cry to your yoga instructor.